Page 123 - JSOM Winter 2017
P. 123
• Cycloplegic eye drop (cyclopentolate 1%), 1 drop
every 8 hours, if available, for photophobia
• Preservative-free artificial tears 3 times per day,
alternating between ointment treatments
Grades II–IV:
• Moxifloxacin 0.5% eye drops, 1 drop every 8
hours Figure 15 Preseptal cellulitis.
• Topical corticosteroid (e.g., tobramycin/dexameth- (http://webeye.ophth.uiowa.edu/
asone or prednisolone acetate 1%) 1 drop every eyeforum/atlas/pages/Preseptal-
hour while awake cellulitis-2.html; reprinted with
permission of The University of
• Cycloplegic drop (cyclopentolate 1%), 1 drop ev- Iowa and EyeRounds.org.)
ery 8 hours, if available
• Doxycycline 100mg PO every 12 hours; this has
anti-inflammatory and anticollagenase benefits
for the ocular surface.
• The following have been shown to improve cor-
neal healing with severe chemical burns; add to Figure 16 Orbital
cellulitis. (©2017
the treatment if available: American Academy of
– Vitamin C 2g 4 times per day. 17 Ophthalmology, reprinted
– Supplemental oxygen (administer 100% for 1 with permission.)
hour twice daily). No data are available for
19
the effectiveness of lower doses of oxygen. o Initiate pain control as needed.
o Reassess frequently until evacuation. o Initiate IV access with broad-spectrum IV antibiotics:
o No altitude restrictions for flight ertapenem 1g IV/IO daily or levofloxacin 500mg IV
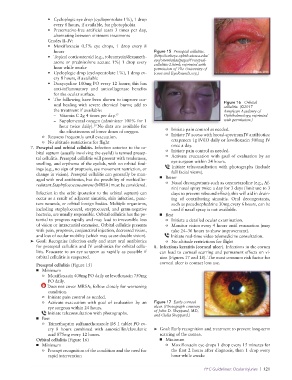
7. Preseptal and orbital cellulitis. Infection anterior to the or- once a day.
bital septum (usually involving the eyelid) is termed presep- o Initiate pain control as needed.
tal cellulitis. Preseptal cellulitis will present with tenderness, o Activate evacuation with goal of evaluation by an
swelling, and erythema of the eyelids, with no orbital find- eye surgeon within 24 hours.
ings (e.g., no sign of proptosis, eye movement restriction, or Initiate teleconsultation with photographs (include
change in vision). Preseptal cellulitis can generally be man- full facial views).
aged with oral antibiotics, but the possibility of methicillin- ■ Better
resistant Staphylococcus aureus (MRSA) must be considered. o Nasal decongestants such as oxymetazoline (e.g., Af-
rin) nasal spray twice a day for 3 days (limit use to 3
Infection in the orbit (posterior to the orbital septum) can days to prevent rebound effect); this will aid in drain-
occur as a result of adjacent sinusitis, skin infection, punc- ing of contributing sinusitis. Oral decongestants,
ture wounds, or orbital foreign bodies. Multiple organisms, such as pseudoephedrine 30mg every 6 hours, can be
including staphylococcal, streptococcal, and gram-negative used if nasal spray is not available.
bacteria, are usually responsible. Orbital cellulitis has the po- ■ Best
tential to progress rapidly and may lead to irreversible loss o Initiate a detailed ocular examination.
of vision or intracranial extension. Orbital cellulitis presents o Monitor vision every 4 hours until evacuation (may
with pain, proptosis, conjunctival injection, decreased vision, take 24–36 hours to show improvement).
and loss of ocular mobility (which may cause double vision). Initiate real-time video telemedicine consultation.
➤ Goal: Recognize infection early and start oral antibiotics o No altitude restrictions for flight
for preseptal cellulitis and IV antibiotics for orbital cellu- 8. Infectious keratitis (corneal ulcer). Infections in the cornea
litis. Evacuate to an eye surgeon as rapidly as possible if can lead to corneal scarring and permanent effects on vi-
orbital cellulitis is suspected. sion (Figures 17 and 18). The most common risk factor for
Preseptal cellulitis (Figure 15) corneal ulcer is contact lens use.
■ Minimum
o Moxifloxacin 400mg PO daily or levofloxacin 750mg
PO daily.
Does not cover MRSA; follow closely for worsening
condition.
o Initiate pain control as needed.
o Activate evacuation with goal of evaluation by an Figure 17 Early corneal
eye surgeon within 24 hours. ulcer. (Photograph courtesy
Initiate teleconsultation with photographs. of John D. Sheppard, MD,
and Clelia Sheppard.)
■ Best
o Trimethoprim sulfamethoxazole DS 1 tablet PO ev-
ery 8 hours combined with amoxicillin/clavulanic ➤ Goal: Early recognition and treatment to prevent long-term
acid 875mg every 12 hours. scarring of the cornea.
Orbital cellulitis (Figure 16) ■ Minimum
■ Minimum o Moxifloxacin eye drops 1 drop every 15 minutes for
o Prompt recognition of the condition and the need for the first 2 hours after diagnosis, then 1 drop every
rapid intervention hour while awake
PFC Guidelines: Ocular Injuries | 121