Page 127 - JSOM Winter 2017
P. 127
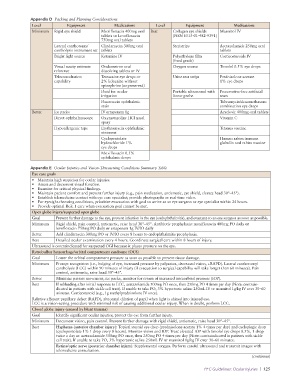
Appendix D Packing and Planning Considerations
Level Equipment Medications Level Equipment Medications
Minimum Rigid eye shield Moxifloxacin 400mg oral Best Collagen eye shields Mannitol IV
tablets or Levofloxacin (NSN 6515-01-482-9391)
750mg oral tablets
Lateral canthotomy/ Clindamycin 300mg oral Steristrips Acetazolamide 250mg oral
cantholysis instrument set tablets tablets
Bright light source Ketamine IV Polyethylene film Corticosteroids IV
(food grade)
Visual acuity estimate Ondansetron oral Oxygen source Timolol 0.5% eye drops
reference dissolving tablets or IV
Teleconsultation Tetracaine eye drops or Urine test strips Prednisolone acetate
capability 2% lidocaine without 1% eye drops
epinephrine (unpreserved)
Fluid for ocular Portable ultrasound with Preservative-free artificial
irrigation linear probe tears
Fluorescein ophthalmic Tobramycin/dexamethasone
stain combination eye drops
Better Ice packs IV ertapenem 1g Acyclovir 400mg oral tablets
Direct ophthalmoscope Oxymetazoline HCl nasal Vitamin C
spray
Hypoallergenic tape Erythromycin ophthalmic Tetanus vaccine
ointment
Cyclopentolate Human rabies immune
hydrochloride 1% globulin and rabies vaccine
eye drops
Moxifloxacin 0.5%
ophthalmic drops
Appendix E Ocular Injuries and Vision-Threatening Conditions Summary Table
Eye care goals
• Maintain high suspicion for ocular injuries.
• Assess and document visual function.
• Examine for critical physical findings.
• Maintain patient comfort and prevent further injury (e.g., pain medication, antiemetic, eye shield, elevate head 30°–45°).
• Establish telemedicine contact with eye care specialist; provide photographs or real-time video.
• For eyesight-threating conditions, prioritize evacuation with goal to arrive at an eye surgeon or eye specialist within 24 hours.
• Provide optimal Role 1 care when evacuation goal cannot be met.
Open globe injury/suspected open globe
Goal Prevent further damage to the eye, prevent infection in the eye (endophthalmitis), and evacuate to an eye surgeon as soon as possible.
Minimum Rigid shield, pain control, antiemetic, raise head 30°–45°. Antibiotic prophylaxis: moxifloxacin 400mg PO daily or
levofloxacin 750mg PO daily or ertapenem 1g IV/IO daily
Better Add clindamycin 300mg PO or IV/IO every 8 hours to endophthalmitis prophylaxis.
Best Detailed ocular examination every 4 hours. Coordinate surgical care within 8 hours of injury.
Ultrasound is contraindicated for suspected OGI because it places pressure on the eye.
Retrobulbar hemorrhage/orbital compartment syndrome (OCS)
Goal Lower the orbital compartment pressure as soon as possible to prevent tissue damage.
Minimum Prompt recognition (i.e., bulging of eye, increased pressure by palpation, decreased vision, +RAPD). Lateral canthotomy/
cantholysis (LCC) within 90 minutes of injury (if evacuation to surgical capability will take longer than 60 minutes). Pain
control, antiemetic, raise head 30°–45°.
Better Minimize patient movement, ice packs, monitor for return of increased intraorbital pressure (IOP).
Best If rebleeding after initial response to LCC, acetazolamide 500mg PO once, then 250mg PO 4 times per day (Note: contrain-
dicated in patients with sickle cell trait). If unable to take PO, 3% hypertonic saline 250mL IV or mannitol 1g/kg IV over 30–60
minutes. Corticosteroid (e.g., 1g methylprednisolone IV once).
Relative afferent pupillary defect (RAPD), abnormal dilation of pupil when light is shined into injured eye.
LCC is a vision-saving procedure with minimal risk of causing additional ocular injury. When in doubt, perform LCC.
Closed globe injury (caused by blunt trauma)
Goal Identify significant ocular injuries; protect the eye from further injury.
Minimum Document vision, pain control. Prevent further damage with rigid shield, antiemetic, raise head 30°–45°.
Best Hyphema (anterior chamber injury): Topical steroid eye drop (prednisolone acetate 1% 4 times per day) and cycloplegic drop
(cyclopentolate 1% 1 drop every 8 hours). Monitor vision and IOP. Treat elevated IOP with timolol eye drops 0.5%, 1 drop
twice a day or acetazolamide 500mg PO once, then 250mg PO 4 times per day (Note: contrain dicated in patients with sickle
cell trait). If unable to take PO, 3% hypertonic saline 250mL IV or mannitol 1g/kg IV over 30–60 minutes.
Retina/optic nerve (posterior chamber injury): Supplemental oxygen. Perform careful ultrasound and transmit images with
telemedicine consultation.
(continues)
PFC Guidelines: Ocular Injuries | 125