Page 29 - 2022 Spring JSOM
P. 29
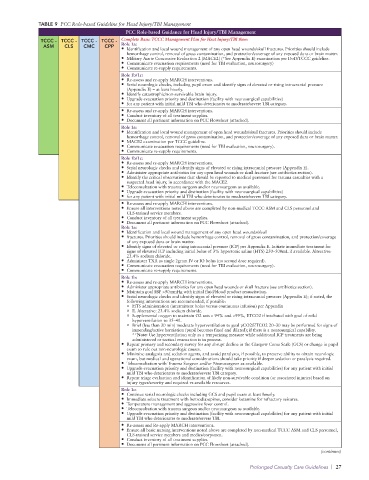
TABLE 9 PCC Role-based Guideline for Head Injury/TBI Management
PCC Role-based Guidance for Head Injury/TBI Management
TCCC - TCCC - TCCC - TCCC - Complete Basic TCCC Management Plan for Heat Injury/TBI then:
ASM CLS CMC CPP Role 1a:
• Identification and local wound management of any open head wounds/skull fractures. Priorities should include
hemorrhage control, removal of gross contamination, and protection/coverage of any exposed dura or brain matter.
• Military Acute Concussive Evaluation 2 (MACE2) (*See Appendix E) examination per DoD/TCCC guideline.
• Communicate evacuation requirements (need for TBI evaluation, neurosurgery)
• Communicate re-supply requirements.
Role 1b/1c:
• Re-assess and re-apply MARCH interventions.
• Serial neurologic checks, including pupil exam and identify signs of elevated or rising intracranial pressure
(Appendix E) – at least hourly.
• Identify catastrophic/non-survivable brain injury.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities)
• for any patient with initial mild TBI who deteriorates to moderate/severe TBI category.
• Re-assess and re-apply MARCH interventions.
• Conduct inventory of all treatment supplies.
• Document all pertinent information on PCC Flowsheet (attached).
Role 1a:
• Identification and local wound management of open head wounds/skull fractures. Priorities should include
hemorrhage control, removal of gross contamination, and protection/coverage of any exposed dura or brain matter.
• MACE2 examination per TCCC guideline.
• Communicate evacuation requirements (need for TBI evaluation, neurosurgery).
• Communicate re-supply requirements.
Role 1b/1c:
• Re-assess and re-apply MARCH interventions.
• Serial neurologic checks and identify signs of elevated or rising intracranial pressure (Appendix E).
• Administer appropriate antibiotics for any open head wounds or skull fracture (see antibiotics section).
• Identify the critical observations that should be reported to medical personnel for trauma casualties with a
suspected head injury, in accordance with the MACE2.
• Teleconsultation with trauma surgeon and/or neurosurgeon as available.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities)
• for any patient with initial mild TBI who deteriorates to moderate/severe TBI category.
• Re-assess and re-apply MARCH interventions.
• Ensure all interventions noted above are completed by non-medical TCCC ASM and CLS personnel and
CLS-trained service members.
• Conduct inventory of all treatment supplies.
• Document all pertinent information on PCC Flowsheet (attached).
Role 1a:
• Identification and local wound management of any open head wounds/skull
• fractures. Priorities should include hemorrhage control, removal of gross contamination, and protection/coverage
of any exposed dura or brain matter.
• Identify signs of elevated or rising intracranial pressure (ICP) per Appendix E. Initiate immediate treatment for
signs of elevated ICP including initial bolus of 3% hypertonic saline (HTS) 250–500mL if available. Alterative:
23.4% sodium chloride.
• Administer TXA as single 2gram IV or IO bolus (no second dose required).
• Communicate evacuation requirements (need for TBI evaluation, neurosurgery).
• Communicate re-supply requirements.
Role 1b:
• Re-assess and re-apply MARCH interventions.
• Administer appropriate antibiotics for any open head wounds or skull fracture (see antibiotics section).
• Maintain goal SBP >90mmHg with initial fluid/blood product resuscitation.
• Serial neurologic checks and identify signs of elevated or rising intracranial pressure (Appendix E); if noted, the
following interventions are recommended, if possible:
o HTS administration (intermittent bolus versus continuous infusion) per Appendix
o E. Alterative: 23.4% sodium chloride.
o Supplemental oxygen to maintain O2 sats > 94% and <99%, ETCO2 if intubated with goal of mild
hyperventilation to 35–40.
o Brief (less than 30 min) moderate hyperventilation to goal pCO2/ETCO2 20–30 may be performed for signs of
impending/active herniation (pupil becomes fixed and dilated); if there is a neurosurgical capability.
**Note: Use hyperventilation only as a temporizing measure while additional ICP treatments are being
administered or tactical evacuation is in process.
• Repeat primary and secondary survey for any abrupt decline in the Glasgow Coma Scale (GCS) or change in pupil
exam to rule out non-neurologic causes.
• Minimize analgesia and sedation agents, and avoid paralyses, if possible, to preserve ability to obtain neurologic
exam, but medical and operational considerations should take priority if deeper sedation or paralysis required.
• Teleconsultation with Trauma Surgeon and/or Neurosurgeon as available.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities) for any patient with initial
mild TBI who deteriorates to moderate/severe TBI category.
• Repeat triage evaluation and identification of likely non-survivable condition (or associated injuries) based on
injury types/severity and required vs available resources.
Role 1c:
• Continue serial neurologic checks including GCS and pupil exam at least hourly.
• Immediate seizure treatment with benzodiazepines, consider ketamine for refractory seizures.
• Temperature management and aggressive fever control.
• Teleconsultation with trauma surgeon and/or neurosurgeon as available.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities) for any patient with initial
mild TBI who deteriorates to moderate/severe TBI.
• Re-assess and Re-apply MARCH interventions.
• Ensure all basic nursing interventions noted above are completed by non-medical TCCC ASM and CLS personnel,
CLS-trained service members and medics/corpsmen.
• Conduct inventory of all treatment supplies.
• Document all pertinent information on PCC Flowsheet (attached).
(continues)
Prolonged Casualty Care Guidelines | 27