Page 25 - 2022 Spring JSOM
P. 25
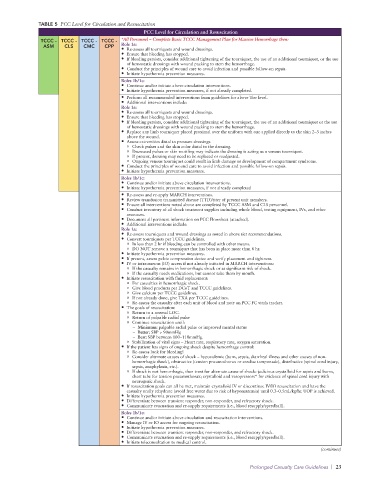
TABLE 5 PCC Level for Circulation and Resuscitation
PCC Level for Circulation and Resuscitation
TCCC - TCCC - TCCC - TCCC - *All Personnel – Complete Basic TCCC Management Plan for Massive Hemorrhage then:
ASM CLS CMC CPP Role 1a:
• Re-assess all tourniquets and wound dressings.
• Ensure that bleeding has stopped.
• If bleeding persists, consider additional tightening of the tourniquet, the use of an additional tourniquet, or the use
of hemostatic dressings with wound packing to stem the hemorrhage.
• Conduct the principles of wound care to avoid infection and possible follow-on sepsis.
• Initiate hypothermia prevention measures.
Roles 1b/1c:
• Continue and/or initiate above circulation interventions.
• Initiate hypothermia prevention measures, if not already completed.
• Perform all recommended interventions from guidelines for above Tier level.
• Additional interventions include:
Role 1a:
• Re-assess all tourniquets and wound dressings.
• Ensure that bleeding has stopped.
• If bleeding persists, consider additional tightening of the tourniquet, the use of an additional tourniquet or the use
of hemostatic dressings with wound packing to stem the hemorrhage.
• Replace any limb tourniquet placed proximal over the uniform with one applied directly to the skin 2–3 inches
above the wound.
• Assess extremities distal to pressure dressings.
o Check pulses and the skin color distal to the dressing.
o Decreased pulses or skin mottling may indicate the dressing is acting as a venous tourniquet.
o If present, dressing may need to be replaced or readjusted.
o Ongoing venous tourniquet could result in limb damage or development of compartment syndrome.
• Conduct the principles of wound care to avoid infection and possible follow-on sepsis.
• Initiate hypothermia prevention measures.
Roles 1b/1c:
• Continue and/or initiate above circulation interventions.
• Initiate hypothermia prevention measures, if not already completed
• Re-assess and re-apply MARCH interventions.
• Review transfusion transmitted disease (TTD)/titer of present unit members.
• Ensure all interventions noted above are completed by TCCC ASM and CLS personnel.
• Conduct inventory of all shock treatment supplies including whole blood, testing equipment, IVs, and other
resources.
• Document all pertinent information on PCC Flowsheet (attached).
• Additional interventions include:
Role 1a:
• Re-assess tourniquets and wound dressings as noted in above tier recommendations.
• Convert tourniquets per TCCC guidelines.
o In less than 2 hr if bleeding can be controlled with other means.
o DO NOT remove a tourniquet that has been in place more than 6 hr.
• Initiate hypothermia prevention measures.
• If present, assess pelvic compression device and verify placement and tightness.
• IV or intraosseous (IO) access if not already initiated in MARCH interventions:
o If the casualty remains in hemorrhagic shock or at significant risk of shock.
o If the casualty needs medications, but cannot take them by mouth.
• Initiate resuscitation with fluid replacement:
o For casualties in hemorrhagic shock.
o Give blood products per DCoT and TCCC guidelines.
o Give calcium per TCCC guidelines.
o If not already done, give TXA per TCCC guidelines.
o Re-assess the casualty after each unit of blood and note on PCC FC vitals tracker.
• The goals of resuscitation:
o Return to a normal LOC.
o Return of palpable radial pulse
o Continue resuscitation until:
– Minimum: palpable radial pulse or improved mental status
– Better: SBP > 90mmHg
– Best: SBP between 100–110mmHg.
o Stabilization of vital signs – Heart rate, respiratory rate, oxygen saturation.
• If the patient has signs of ongoing shock despite hemorrhage control:
o Re-assess look for bleeding!
o Consider alternate causes of shock – hypovolemic (burn, sepsis, diarrheal illness and other causes of non-
hemorrhagic shock), obstructive (tension pneumothorax or cardiac tamponade), distributive (spinal cord injury,
sepsis, anaphylaxis, etc.).
o If shock is not hemorrhagic, then treat for alternate cause of shock: judicious crystalloid for sepsis and burns,
chest tube for tension pneumothorax; crystalloid and vasopressors* for evidence of spinal cord injury with
neurogenic shock.
• If resuscitation goals can all be met, maintain crystalloid IV or discontinue IV/IO resuscitation and have the
casualty orally rehydrate (avoid free water due to risk of hyponatremia) until 0.3–0.5mL/kg/hr. UOP is achieved.
• Initiate hypothermia prevention measures.
• Differentiate between transient responder, non-responder, and refractory shock.
• Communicate evacuation and re-supply requirements (i.e., blood resupply/speedball).
Roles 1b/1c:
• Continue and/or initiate above circulation and resuscitation interventions.
• Manage IV or IO access for ongoing resuscitation.
• Initiate hypothermia prevention measures.
• Differentiate between transient responder, non-responder, and refractory shock.
• Communicate evacuation and re-supply requirements (i.e., blood resupply/speedball).
• Initiate teleconsultation to medical control.
(continues)
Prolonged Casualty Care Guidelines | 23