Page 24 - 2022 Spring JSOM
P. 24
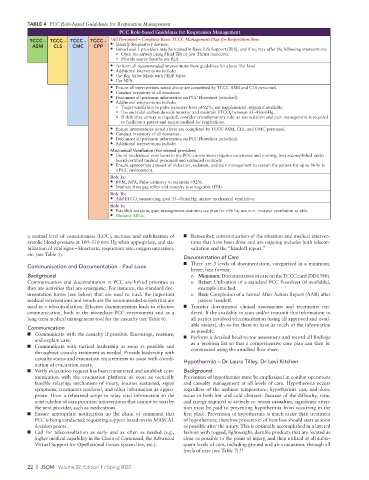
TABLE 4 PCC Role-based Guidelines for Respiration Management
PCC Role-based Guidelines for Respiration Management
TCCC - TCCC - TCCC - TCCC - *All Personnel – Complete Basic TCCC Management Plan for Respiration then:
ASM CLS CMC CPP • Identify Respiratory distress.
• Some Level 1 providers may be trained in Basic Life Support (BLS), and if so, may offer the following interventions:
o Open the airway using Head Tilt or Jaw Thrust maneuver.
o Provide rescue breaths per BLS.
• Perform all recommended interventions from guidelines for above Tier level
• Additional interventions include:
• Use Bag Valve Mask with PEEP Valve.
• Use NPA.
• Ensure all interventions noted above are completed by TCCC ASM and CLS personnel.
• Conduct inventory of all resources.
• Document all pertinent information on PCC Flowsheet (attached).
• Additional interventions include:
o Target ventilation to pulse oximetry level of 92%; use supplemental oxygen if available.
o Use end-tidal carbon dioxide monitor and maintain ETCO between 35–45mmHg.
2
o If definitive airway is required, consider cricothyrotomy tube as less sedation and pain management is required
to facilitate a patent and secure method for respirations.
• Ensure interventions noted above are completed by TCCC ASM, CLS, and CMC personnel.
• Conduct inventory of all resources.
• Document all pertinent information on PCC Flowsheet (attached).
• Additional interventions include:
Mechanical Ventilation (For trained providers)
• Use of mechanical ventilators in the PCC environment requires experience and training, best accomplished under
board-certified medical personnel and sustained routinely.
• Ensure appropriate amount of induction, sedation, and pain management to sustain the patient for up to 96 hr in
a PCC environment.
Role 1a:
• BVM, NPA, Pulse oximetry to maintain >92%.
• Intubate if no gag reflex and casualty is salvageable (TBI).
Role 1b:
• Add ETCO monitoring, goal 35–45mmHg; initiate mechanical ventilation.
2
Role 1c:
• Establish sedation, pain management maintenance plan for >96 hr; use non- invasive ventilation as able.
• Monitor ABGs.
a normal level of consciousness (LOC), increase and stabilization of ■ Remember, communication of the situation and medical interven-
systolic blood pressure at 100–110 mm Hg when appropriate, and sta- tions that have been done and are ongoing includes both telecon-
bilization of vital signs – Heart rate, respiratory rate, oxygen saturation, sultation and the “handoff report.”
etc. (see Table 5).
Documentation of Care
■ There are 3 levels of documentation, categorized in a minimum,
Communication and Documentation - Paul Loos
better, best format:
Background o Minimum: Documentation of care on the TCCC card (DD1380).
Communication and documentation in PCC are linked priorities as o Better: Utilization of a standard PCC flowsheet (if available),
they are activities that are synergistic. For instance, the standard doc- example attached.
umentation forms (see below) that are used to track the important o Best: Completion of a formal After Action Report (AAR) after
medical interventions and trends are the recommended scripts that are patient handoff.
used in a teleconsultation. Effective documentation leads to effective ■ Transfer documented clinical assessments and treatments ren-
communication, both in the immediate PCC environment and as a dered. If the availably to scan and/or transmit this information to
long-term medical management tool for the casualty (see Table 6). all parties involved teleconsultation (using all approved and avail-
able means), do so for them to have as much of the information
Communication as possible.
■ Communicate with the casualty if possible. Encourage, reassure, ■ Perform a detailed head-to-toe assessment and record all findings
and explain care.
■ Communicate with tactical leadership as soon as possible and as a problem list so that a comprehensive care plan can then be
constructed using the attached flow sheet.
throughout casualty treatment as needed. Provide leadership with
casualty status and evacuation requirements to assist with coordi-
nation of evacuation assets. Hypothermia – Dr Laura Tilley, Dr Levi Kitchen
■ Verify evacuation request has been transmitted and establish com- Background
munication with the evacuation platform as soon as tactically Prevention of hypothermia must be emphasized in combat operations
feasible relaying: mechanism of injury, injuries sustained, signs/ and casualty management at all levels of care. Hypothermia occurs
symptoms, treatments rendered, and other information as appro- regardless of the ambient temperature; hypothermia can, and does,
priate. Have a rehearsed script to relay vital information to the occur in both hot and cold climates. Because of the difficulty, time,
next echelon of care prioritize interventions that cannot be seen by and energy required to actively re- warm casualties, significant atten-
the next provider, such as medications. tion must be paid to preventing hypothermia from occurring in the
■ Ensure appropriate notification up the chain of command that first place. Prevention of hypothermia is much easier than treatment
PCC is being conducted; requesting support based on the MASCAL of hypothermia; therefore prevention of heat loss should start as soon
decision points. as possible after the injury. This is optimally accomplished in a layered
■ Call for teleconsultation as early and as often as needed (e.g., fashion with rugged, lightweight, durable products that are located as
higher medical capability in the Chain of Command, the Advanced close as possible to the point of injury, and then utilized at all subse-
VIrtual Support for OpeRational Forces system line, etc.). quent levels of care, including ground and air evacuation, through all
levels of care (see Table 7). 12
22 | JSOM Volume 22, Edition 1 / Sping 2022