Page 30 - 2022 Spring JSOM
P. 30
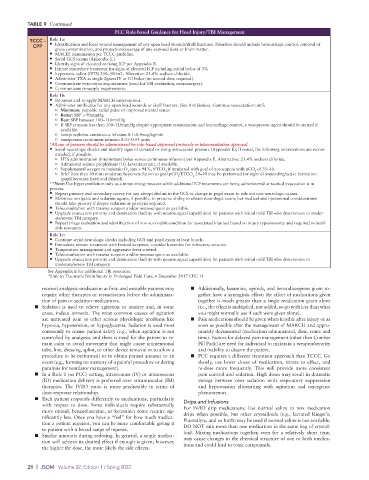
TABLE 9 Continued
PCC Role-based Guidance for Head Injury/TBI Management
TCCC - Role 1a:
CPP • Identification and local wound management of any open head wounds/skull fractures. Priorities should include hemorrhage control, removal of
gross contamination, and protection/coverage of any exposed dura or brain matter.
• MACE2 examination per TCCC guideline.
• Serial GCS exams (Appendix E.)
• Identify signs of elevated or rising ICP per Appendix E.
• Initiate immediate treatment for signs of elevated ICP including initial bolus of 3%
• hypertonic saline (HTS) 250–500mL. Alterative: 23.4% sodium chloride.
• Administer TXA as single 2gram IV or IO bolus (no second dose required).
• Communicate evacuation requirements (need for TBI evaluation, neurosurgery).
• Communicate re-supply requirements.
Role 1b:
• Re-assess and re-apply MARCH interventions.
• Administer antibiotics for any open head wounds or skull fracture. (See Antibiotics). Continue resuscitation until:
o Minimum: palpable radial pulse or improved mental status
o Better: SBP > 90mmHg
o Best: SBP between 100–110mmHg
o If SBP remains less than 100–110mmHg despite appropriate resuscitation and hemorrhage control, a vasopressor agent should be started if
available.
o norepinephrine continuous infusion 0.1–0.4mcg/kg/min
o vasopressin continuous infusion 0.01–0.04 units
*All use of pressers should be administered by role-based approved protocols or teleconsultation approval
• Serial neurologic checks and identify signs of elevated or rising intracranial pressure (Appendix E); If noted, the following interventions are recom-
mended, if possible:
o HTS administration (intermittent bolus versus continuous infusion) per Appendix E. Alternative: 23.4% sodium chloride.
o Administer seizure prophylaxis (1G Levetiracetam), if available.
o Supplemental oxygen to maintain O sats > 94%, ETCO if intubated with goal of norocapnia with pCO of 35–40.
2
2
2
o Brief (less than 30 min) moderate hyperventilation to goal pCO /ETCO 20–30 may be performed for signs of impending/active herniation
2
2
(pupil becomes fixed and dilated).
**Note: Use hyperventilation only as a temporizing measure while additional ICP treatments are being administered or tactical evacuation is in
process.
• Repeat primary and secondary survey for any abrupt decline in the GCS or change in pupil exam to rule out non-neurologic causes.
• Minimize analgesia and sedation agents, if possible, to preserve ability to obtain neurologic exam, but medical and operational considerations
should take priority if deeper sedation or paralysis required.
• Teleconsultation with trauma surgeon and/or neurosurgeon as available.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities) for patients with initial mild TBI who deteriorates to moder-
ate/severe TBI category.
• Repeat triage evaluation and identification of non-survivable condition (or associated injuries) based on injury types/severity and required vs avail-
able resources.
Role 1c:
• Continue serial neurologic checks including GCS and pupil exam at least hourly.
• Immediate seizure treatment with benzodiazepines, consider ketamine for refractory seizures.
• Temperature management and aggressive fever control.
• Teleconsultation with trauma surgeon and/or neurosurgeon as available.
• Upgrade evacuation priority and destination (facility with neurosurgical capabilities) for patients with initial mild TBI who deteriorates to
moderate/severe TBI category.
See Appendix E for additional TBI resources.
*Link to Traumatic Brain Injury in Prolonged Field Care, 6 December 2017 CPG 14
receive) analgesic medication at first, and unstable patients may ■ Additionally, ketamine, opioids, and benzodiazepines given to-
require other therapies or resuscitation before the administra- gether have a synergistic effect: the effect of medications given
tion of pain or sedation medications. together is much greater than a single medication given alone
■ Sedation is used to relieve agitation or anxiety and, in some (i.e., the effect is multiplied, not added, so go with less than what
cases, induce amnesia. The most common causes of agitation you might normally use if each were given alone).
are untreated pain or other serious physiologic problems like ■ Pain medications should be given when feasible after injury or as
hypoxia, hypotension, or hypoglycemia. Sedation is used most soon as possible after the management of MARCH and appro-
commonly to ensure patient safety (e.g., when agitation is not priately documented (medication administered, dose, route and
controlled by analgesia and there is need for the patient to re- time). Factors for delayed pain management (other than Combat
main calm to avoid movement that might cause unintentional Pill Pack) are need for individual to maintain a weapon/security
tube, line, dressing, splint, or other device removal or to allow a and inability to disarm the patient.
procedure to be performed) or to obtain patient amnesia to an ■ PCC requires a different treatment approach than TCCC. Go
event (e.g., forming no memory of a painful procedure or during slowly, use lower doses of medication, titrate to effect, and
paralysis for ventilator management). re-dose more frequently. This will provide more consistent
■ In a Role 1 (or PCC) setting, intravenous (IV) or interosseous pain control and sedation. High doses may result in dramatic
(IO) medication delivery is preferred over intramuscular (IM) swings between over sedation with respiratory suppression
therapies. The IV/IO route is more predictable in terms of and hypotension alternating with agitation and emergence
dose-response relationship. phenomenon.
■ Each patient responds differently to medications, particularly Drips and Infusions
with respect to dose. Some individuals require substantially For IV/IO drip medications: Use normal saline to mix medication
more opioid, benzodiazepine, or ketamine; some require sig- drips when possible, but other crystalloids (e.g., lactated Ringer’s,
nificantly less. Once you have a “feel” for how much medica- Plasmalyte, and so forth) may be used if normal saline is not available.
tion a patient requires, you can be more comfortable giving it DO NOT mix more than one medication in the same bag of crystal-
to patient with a broad range of injuries.
■ Similar amounts during redosing. In general, a single medica- loid. Mixing medications together, even for a relatively short time,
may cause changes to the chemical structure of one or both medica-
tion will achieve its desired effect if enough is given; however, tions and could lead to toxic compounds.
the higher the dose, the more likely the side effects.
28 | JSOM Volume 22, Edition 1 / Sping 2022