Page 31 - 2022 Spring JSOM
P. 31
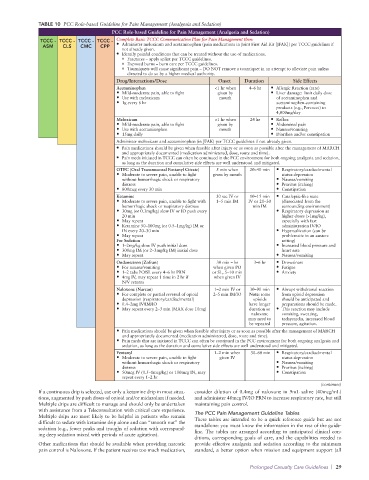
TABLE 10 PCC Role-based Guideline for Pain Management (Analgesia and Sedation)
PCC Role-based Guideline for Pain Management (Analgesia and Sedation)
TCCC - TCCC - TCCC - TCCC - Complete Basic TCCC Communication Plan for Pain Management then:
ASM CLS CMC CPP • Administer meloxicam and acetaminophen (pain medications in Joint First Aid Kit [JFAK]) per TCCC guidelines if
not already given.
• Identify painful conditions that can be treated without the use of medications.
o Fractures – apply splint per TCCC guidelines.
o Exposed burns – burn care per TCCC guidelines.
o Tourniquets will cause significant pain – DO NOT remove a tourniquet in an attempt to alleviate pain unless
directed to do so by a higher medical authority.
Drug/Interactions/Dose Onset Duration Side Effects
Acetaminophen <1 hr when 4–6 hr • Allergic Reaction (rare)
• Mild-moderate pain, able to fight given by • Liver damage: limit daily dose
• Use with meloxicam mouth of acetaminophen and
• 1g every 6 hr acetaminophen-containing
products (e.g., Percocet) to
4,000mg/day
Meloxicam <1 hr when 24 hr • Reflux
• Mild-moderate pain, able to fight given by • Abdominal pain
• Use with acetaminophen mouth • Nausea/vomiting
• 15mg daily • Diarrhea and/or constipation
Administer meloxicam and acetaminophen (in JFAK) per TCCC guidelines if not already given.
• Pain medications should be given when feasible after injury or as soon as possible after the management of MARCH
and appropriately documented (medication administered, dose, route and time).
• Pain meds initiated in TCCC can often be continued in the PCC environment for both ongoing analgesia and sedation,
as long as the duration and cumulative side effects are well understood and mitigated.
OTFC (Oral Transmucosal Fentanyl Citrate) 5 min when 20–40 min • Respiratory/cardiac/mental
• Moderate to severe pain, unable to fight given by mouth status depression
without hemorrhagic shock or respiratory • Nausea/vomiting
distress • Pruritus (itching)
• 800mcg every 30 min • Constipation
Ketamine 30 sec IV or 10–15 min • Cataleptic-like state
• Moderate to severe pain, unable to fight with 1–5 min IM IV or 20–30 (dissociated from the
hemorrhagic shock or respiratory distress min IM surrounding environment)
• 30mg (or 0.3mg/kg) slow IV or IO push every • Respiratory depression at
20 min higher doses (>1mg/kg),
• May repeat especially with fast
• Ketamine 50–100mg (or 0.5–1mg/kg) IM or administration IV/IO
IN every 20–30 min • Hypersalivation (can be
• May repeat problematic in an austere
For Sedation setting)
• 1–2mg/kg slow IV push initial dose • Increased blood pressure and
• 300mg IM (or 2–3mg/kg IM) initial dose heart rate
• May repeat • Nausea/vomiting
Ondansetron (Zofran) 30 min – hr 3–6 hr • Drowsiness
• For nausea/vomiting when given PO • Fatigue
• 1–2 tabs PO/SL every 4–6 hr PRN or SL, 5–10 min • Anxiety
• 4mg IV, may repeat 1 time in 2 hr if when given IV
N/V returns
Naloxone (Narcan) 1–2 min IV or 30–90 min • Abrupt withdrawal reaction
• For complete or partial reversal of opioid 2–5 min IM/IO Note: some from opioid depression
depression (respiratory/cardiac/mental) opioids should be anticipated and
• 0.4–2mg IV/IM/IO have longer preparations should be made.
• May repeat every 2–3 min (MAX dose 10mg) duration so • This reaction may include
naloxone vomiting, sweating,
may need to tachycardia, increased blood
be repeated pressure, agitation.
• Pain medications should be given when feasible after injury or as soon as possible after the management of MARCH
and appropriately documented (medication administered, dose, route and time).
• Pain meds that are initiated in TCCC can often be continued in the PCC environment for both ongoing analgesia and
sedation, as long as the duration and cumulative side effects are well understood and mitigated.
Fentanyl 1–2 min when 30–60 min • Respiratory/cardiac/mental
• Moderate to severe pain, unable to fight given IV status depression
without hemorrhagic shock or respiratory • Nausea/vomiting
distress • Pruritus (itching)
• 50mcg IV (0.5–1mcg/kg) or 100mcg IN, may • Constipation
repeat every 1–2 hr
(continues)
If a continuous drip is selected, use only a ketamine drip in most situa- consider dilution of 0.4mg of naloxone in 9mL saline (40mcg/mL)
tions, augmented by push doses of opioid and/or midazolam if needed. and administer 40mcg IV/IO PRN to increase respiratory rate, but still
Multiple drips are difficult to manage and should only be undertaken maintaining pain control.
with assistance from a Teleconsultation with critical care experience. The PCC Pain Management Guideline Tables
Multiple drips are most likely to be helpful in patients who remain These tables are intended to be a quick reference guide but are not
difficult to sedate with ketamine drip alone and can “smooth out” the standalone: you must know the information in the rest of the guide-
sedation (e.g., fewer peaks and troughs of sedation with correspond- line. The tables are arranged according to anticipated clinical con-
ing deep sedation mixed with periods of acute agitation).
ditions, corresponding goals of care, and the capabilities needed to
Other medications that should be available when providing narcotic provide effective analgesia and sedation according to the minimum
pain control is Naloxone. If the patient receives too much medication, standard, a better option when mission and equipment support (all
Prolonged Casualty Care Guidelines | 29