Page 24 - Journal of Special Operations Medicine - Spring 2016
P. 24
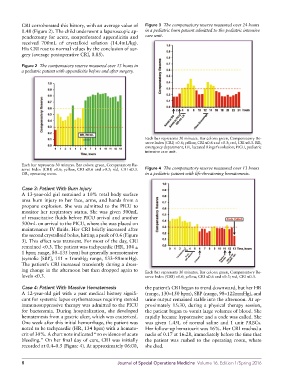
CRI corroborated this history, with an average value of Figure 3 The compensatory reserve measured over 24 hours
0.48 (Figure 2). The child underwent a laparoscopic ap- in a pediatric burn patient admitted to the pediatric intensive
pendectomy for acute, nonperforated appendicitis and care unit.
received 700mL of crystalloid solution (14.4mL/kg).
His CRI rose to normal values by the conclusion of sur-
gery (average postoperative CRI, 0.85).
Figure 2 The compensatory reserve measured over 13 hours in
a pediatric patient with appendicitis before and after surgery.
Each bar represents 30 minutes. Bar colors: green, Compensatory Re-
serve Index (CRI) >0.6; yellow, CRI ≤0.6 and >0.3; red, CRI ≤0.3. ED,
emergency department; LR, lactated Ringer’s solution; PICU, pediatric
intensive care unit.
Each bar represents 30 minutes. Bar colors: green, Compensatory Re-
serve Index (CRI) >0.6; yellow, CRI ≤0.6 and >0.3; red, CRI ≤0.3. Figure 4 The compensatory reserve measured over 13 hours
OR, operating room. in a pediatric patient with life-threatening hematemesis.
Case 3: Patient With Burn Injury
A 13-year-old girl sustained a 10% total body surface
area burn injury to her face, arms, and hands from a
propane explosion. She was admitted to the PICU to
monitor her respiratory status. She was given 500mL
of resuscitative fluids before PICU arrival and another
500mL on arrival to the PICU, where she was placed on
maintenance IV fluids. Her CRI briefly increased after
the second crystalloid bolus, hitting a peak of 0.6 (Figure
3). This effect was transient. For most of the day, CRI
remained <0.3. The patient was tachycardic (HR, 104 ±
1 bpm; range, 80–135 bpm) but generally normotensive
(systolic [SBP], 111 ± 1mmHg; range, 133–88mmHg).
The patient’s CRI increased transiently during a dress-
ing change in the afternoon but then dropped again to Each bar represents 30 minutes. Bar colors: green, Compensatory Re-
levels <0.3. serve Index (CRI) >0.6; yellow, CRI ≤0.6 and >0.3; red, CRI ≤0.3.
Case 4: Patient With Massive Hematemesis the patient’s CRI began to trend downward, but her HR
A 12-year-old girl with a past medical history signifi- (range, 130–150 bpm), SBP (range, 98–122mmHg), and
cant for systemic lupus erythematosus requiring steroid urine output remained stable into the afternoon. At ap-
immunosuppressive therapy was admitted to the PICU proximately 15:30, during a physical therapy session,
for bacteremia. During hospitalization, she developed the patient began to vomit large volumes of blood. She
hematemesis from a gastric ulcer, which was cauterized. rapidly became hypotensive and a code was called. She
One week after this initial hemorrhage, the patient was was given 1.45L of normal saline and 1 unit PRBCs.
noted to be tachycardic (HR, 134 bpm) with a hemato- Her follow-up hematocrit was 16%. Her CRI reached a
crit of 30%. A chart note indicated “no evidence of acute nadir of 0.17 at 16:28, immediately before the time that
bleeding.” On her final day of care, CRI was initially the patient was rushed to the operating room, where
recorded at 0.4–0.5 (Figure 4). At approximately 06:00, she died.
8 Journal of Special Operations Medicine Volume 16, Edition 1/Spring 2016