Page 65 - Journal of Special Operations Medicine - Spring 2017
P. 65
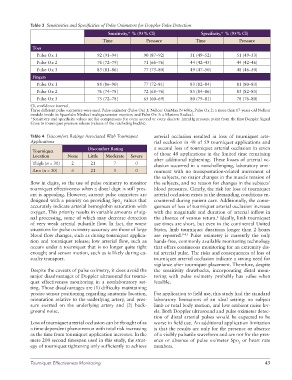
Table 3 Sensitivities and Specificities of Pulse Oximeters for Doppler Pulse Detection
Sensitivity,* % (95% CI) Specificity,* % (95% CI)
Time Pressure Time Pressure
Toes
Pulse Ox 1 92 (91–94) 90 (87–92) 51 (49–52) 51 (49–53)
Pulse Ox 2 76 (72–79) 71 (66–76) 44 (42–45) 44 (42–46)
Pulse Ox 3 83 (81–86) 77 (73–80) 49 (47–50) 48 (46–50)
Fingers
Pulse Ox 1 88 (86–90) 77 (72–81) 83 (82–84) 81 (80–83)
Pulse Ox 2 76 (74–78) 72 (68–76) 85 (84–86) 83 (82–85)
Pulse Ox 3 75 (72–78) 65 (60–69) 80 (79–81) 78 (76–80)
CI, confidence interval.
Three different pulse oximeters were used. Pulse oximeter (Pulse Ox) 1: Nellcor OxiMax N-600x; Pulse Ox 2: a more than 17-years-old Nellcor
module inside its Spacelabs Medical multiparameter monitor; and Pulse Ox 3: a Masimo Radical.
*Sensitivity and specificity values are for comparisons for every second or every discrete 1mmHg pressure point from the first Doppler Signal
Gone to tourniquet pressure release (release of the ratcheting buckle).
Table 4 Discomfort Ratings Associated With Tourniquet arterial occlusion resulted in loss of tourniquet arte-
Applications rial occlusion in 48 of 59 tourniquet applications and
Discomfort Rating a second loss of tourniquet arterial occlusion in seven
Tourniquet of those 48 applications in the limited time remaining
Location None Little Moderate Severe
after additional tightening. These losses of arterial oc-
Thigh (n = 30) 2 21 7 0
clusion occurred in a nonchallenging, laboratory envi-
Arm (n = 30) 6 21 3 0 ronment with no transportation-related movement of
the subjects, no major changes in the muscle tension of
flow in digits, so the use of pulse oximetry to monitor the subjects, and no reason for changes in the subjects’
tourniquet effectiveness when a distal digit is still pres- blood pressures. Clearly, the risk for loss of tourniquet
ent is appealing. However, current pulse oximeters are arterial occlusion exists in the demanding conditions en-
designed with a priority on providing Spo values that countered during patient care. Additionally, the conse-
2
accurately indicate arterial hemoglobin saturation with quences of loss of tourniquet arterial occlusion increase
oxygen. This priority results in variable amounts of sig- with the magnitude and duration of arterial inflow in
nal processing, some of which may decrease detection the absence of venous return. Ideally, limb tourniquet
2
of very weak arterial pulsatile flow. In fact, the worst use times are short, but even in the continental United
situations for pulse oximetry accuracy are those of large States, limb tourniquet durations longer than 2 hours
blood flow changes, such as during tourniquet applica- are reported. 9–13 Pulse oximetry is currently the only
tion and tourniquet release; low arterial flow, such as hands-free, commonly available monitoring technology
occurs under a tourniquet that is no longer quite tight that offers continuous monitoring for an extremity dis-
enough; and sensor motion, such as is likely during ca- tal arterial pulse. The risks and consequences of loss of
sualty transport. tourniquet arterial occlusion indicate a strong need for
vigilance after tourniquet placement. Therefore, despite
Despite the caveats of pulse oximetry, it does avoid the the sensitivity drawbacks, incorporating distal moni-
major disadvantages of Doppler ultrasound for tourni- toring with pulse oximetry probably has value when
quet effectiveness monitoring in a nonlaboratory set- feasible.
ting. Those disadvantages are (1) difficulty maintaining
precise sensor positioning regarding anatomic location, For application to field use, this study had the standard
orientation relative to the underlying artery, and pres- laboratory limitations of an ideal setting: no subject
sure exerted on the underlying artery and (2) back- limb or total body motion, and low ambient noise lev-
ground noise. els. Both Doppler ultrasound and pulse oximeter detec-
tion of distal arterial pulses would be expected to be
Loss of tourniquet arterial occlusion can be thought of as worse in field use. An additional application limitation
a time-dependent phenomenon with total risk increasing is that the results are only for the presence or absence
as the time from tourniquet application increases. In the of a visibly pulsatile waveform and are not for the pres-
mere 200 second timespan used in this study, the strat- ence or absence of pulse oximeter Spo or heart rate
2
egy of tourniquet tightening only sufficiently to achieve numbers.
Tourniquet Effectiveness Monitoring 43