Page 83 - JSOM Fall 2024
P. 83
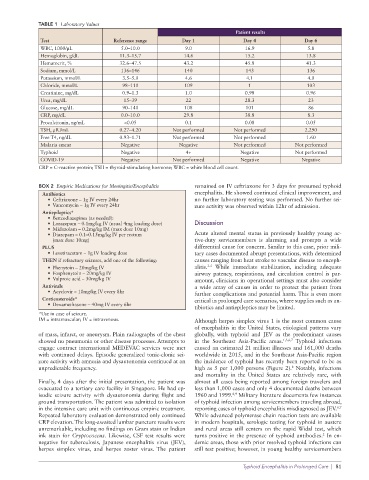
TABLE 1 Laboratory Values
Patient results
Test Reference range Day 1 Day 4 Day 6
WBC, 1000/μL 5.0–10.0 9.0 16.9 5.8
Hemoglobin, g/dL 11.3–15.7 14.6 15.2 13.8
Hematocrit, % 32.6–47.5 43.2 45.8 41.3
Sodium, mmol/L 136–146 140 143 136
Potassium, mmol/L 3.5–5.0 4.6 4.1 4.0
Chloride, mmol/L 98–110 109 1 103
Creatinine, mg/dL 0.9–1.3 1.0 0.98 0.96
Urea, mg/dL 15–39 22 28.3 23
Glucose, mg/dL 90–140 108 101 86
CRP, mg/dL 0.0–10.0 29.8 38.8 8.3
Procalcitonin, ng/mL <0.05 0.1 0.08 0.05
TSH, μIU/mL 0.27–4.20 Not performed Not performed 2.290
Free T4, ng/dL 0.93–1.71 Not performed Not performed 1.60
Malaria smear Negative Negative Not performed Not performed
Typhoid Negative 4+ Negative Not performed
COVID-19 Negative Not performed Negative Negative
CRP = C-reactive protein; TSH = thyroid-stimulating hormone; WBC = white blood cell count.
BOX 2 Empiric Medications for Meningitis/Encephalitis remained on IV ceftriaxone for 3 days for presumed typhoid
Antibiotics encephalitis. He showed continued clinical improvement, and
• Ceftriaxone – 1g IV every 24hr no further laboratory testing was performed. No further sei-
• Vancomycin – 1g IV every 24hr zure activity was observed within 12hr of admission.
Antiepileptics*
• Benzodiazepines (as needed):
• Lorazepam – 0.1mg/kg IV (usual 4mg loading dose) Discussion
• Midazolam – 0.2mg/kg IM (max dose 10mg)
• Diazepam – 0.1–0.15mg/kg IV per rectum Acute altered mental status in previously healthy young ac-
(max dose 10mg) tive-duty servicemembers is alarming and prompts a wide
PLUS differential cause for concern. Similar to this case, prior mili-
• Levetiracetam – 1g IV loading dose tary cases documented abrupt presentations, with determined
THEN if refractory seizures, add one of the following: causes ranging from heat stroke to vascular disease to enceph-
3-5
• Phenytoin – 20mg/kg IV alitis. While immediate stabilization, including adequate
• Fosphenytoin – 20mg/kg IV airway patency, respirations, and circulation control is par-
• Valproic acid – 30mg/kg IV amount, clinicians in operational settings must also consider
Antivirals a wide array of causes in order to protect the patient from
• Acyclovir – 10mg/kg IV every 8hr further complications and potential harm. This is even more
Corticosteroids* critical in prolonged care scenarios, where supplies such as an-
• Dexamethasone – 40mg IV every 6hr
tibiotics and antiepileptics may be limited.
*Use in case of seizure.
IM = intramuscular; IV = intravenous. Although herpes simplex virus 1 is the most common cause
of encephalitis in the United States, etiological patterns vary
of mass, infarct, or aneurysm. Plain radiographs of the chest globally, with typhoid and JEV as the predominant causes
showed no pneumonia or other disease processes. Attempts to in the Southeast Asia-Pacific areas. 1,3,6,7 Typhoid infections
engage contract international MEDEVAC services were met caused an estimated 21 million illnesses and 161,000 deaths
with continued delays. Episodic generalized tonic-clonic sei- worldwide in 2015, and in the Southeast Asia-Pacific region
zure activity with amnesia and dysautonomia continued at an the incidence of typhoid has recently been reported to be as
8
unpredictable frequency. high as 5 per 1,000 persons (Figure 2). Notably, infections
and mortality in the United States are relatively rare, with
Finally, 4 days after the initial presentation, the patient was almost all cases being reported among foreign travelers and
evacuated to a tertiary care facility in Singapore. He had ep- less than 1,000 cases and only 4 documented deaths between
isodic seizure activity with dysautonomia during flight and 1960 and 1999. Military literature documents few instances
8,9
ground transportation. The patient was admitted to isolation of typhoid infection among servicemembers traveling abroad,
6,7
in the intensive care unit with continuous empiric treatment. reporting cases of typhoid encephalitis misdiagnosed as JEV.
Repeated laboratory evaluation demonstrated only continued While advanced polymerase chain reaction tests are available
CRP elevation. The long-awaited lumbar puncture results were in modern hospitals, serologic testing for typhoid in austere
unremarkable, including no findings on Gram stain or Indian and rural areas still centers on the rapid Widal test, which
2
ink stain for Cryptococcus. Likewise, CSF test results were turns positive in the presence of typhoid antibodies. In en-
negative for tuberculosis, Japanese encephalitis virus (JEV), demic areas, those with prior resolved typhoid infections can
herpes simplex virus, and herpes zoster virus. The patient still test positive; however, in young healthy servicemembers
Typhoid Encephalitis in Prolonged Care | 81