Page 82 - JSOM Fall 2024
P. 82
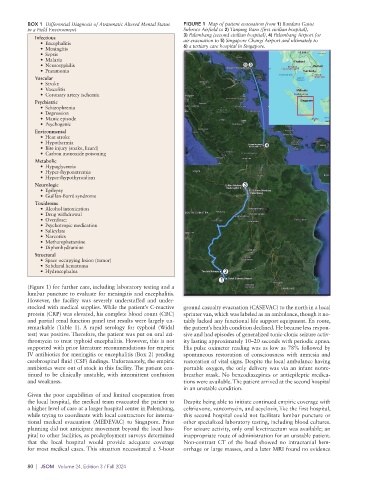
BOX 1 Differential Diagnosis of Atraumatic Altered Mental Status FIGURE 1 Map of patient evacuation from 1) Bandara Gatot
in a Field Environment Subroto Airfield to 2) Tanjung Baru (first civilian hospital),
Infectious 3) Palembang (second civilian hospital), 4) Palembang Airport for
air evacuation to 5) Singapore Changi Airport and ultimately to
• Encephalitis 6) a tertiary care hospital in Singapore.
• Meningitis
• Sepsis
• Malaria
• Neurosyphilis
• Pneumonia
Vascular
• Stroke
• Vasculitis
• Coronary artery ischemia
Psychiatric
• Schizophrenia
• Depression
• Manic episode
• Psychogenic
Environmental
• Heat stroke
• Hypothermia
• Bite injury (snake, lizard)
• Carbon monoxide poisoning
Metabolic
• Hypoglycemia
• Hyper-/hyponatremia
• Hyper-/hypothyroidism
Neurologic
• Epilepsy
• Guillan-Barré syndrome
Toxidrome
• Alcohol intoxication
• Drug withdrawal
• Overdose:
• Psychotropic medication
• Salicylate
• Narcotics
• Methamphetamine
• Diphenhydramine
Structural
• Space occupying lesion (tumor)
• Subdural hematoma
• Hydrocephalus
(Figure 1) for further care, including laboratory testing and a
lumbar puncture to evaluate for meningitis and encephalitis.
However, the facility was severely understaffed and under-
stocked with medical supplies. While the patient’s C-reactive ground casualty evacuation (CASEVAC) to the north in a local
protein (CRP) was elevated, his complete blood count (CBC) sprinter van, which was labeled as an ambulance, though it no-
and partial renal function panel test results were largely un- tably lacked any functional life support equipment. En route,
remarkable (Table 1). A rapid serology for typhoid (Widal the patient’s health condition declined. He became less respon-
test) was positive. Therefore, the patient was put on oral azi- sive and had episodes of generalized tonic-clonic seizure activ-
thromycin to treat typhoid encephalitis. However, this is not ity lasting approximately 10–20 seconds with periodic apnea.
supported with prior literature recommendations for empiric His pulse oximeter reading was as low as 78% followed by
IV antibiotics for meningitis or encephalitis (Box 2) pending spontaneous restoration of consciousness with amnesia and
cerebrospinal fluid (CSF) findings. Unfortunately, the empiric restoration of vital signs. Despite the local ambulance having
antibiotics were out of stock in this facility. The patient con- portable oxygen, the only delivery was via an infant nonre-
tinued to be clinically unstable, with intermittent confusion breather mask. No benzodiazepines or antiepileptic medica-
and weakness. tions were available. The patient arrived at the second hospital
in an unstable condition.
Given the poor capabilities of and limited cooperation from
the local hospital, the medical team evacuated the patient to Despite being able to initiate continued empiric coverage with
a higher level of care at a larger hospital center in Palembang, ceftriaxone, vancomycin, and acyclovir, like the first hospital,
while trying to coordinate with local contractors for interna- this second hospital could not facilitate lumbar puncture or
tional medical evacuation (MEDEVAC) to Singapore. Prior other specialized laboratory testing, including blood cultures.
planning did not anticipate movement beyond the local hos- For seizure activity, only oral levetiracetam was available; an
pital to other facilities, as predeployment surveys determined inappropriate route of administration for an unstable patient.
that the local hospital would provide adequate coverage Non-contrast CT of the head showed no intracranial hem-
for most medical cases. This situation necessitated a 5-hour orrhage or large masses, and a later MRI found no evidence
80 | JSOM Volume 24, Edition 3 / Fall 2024