Page 37 - 2022 Spring JSOM
P. 37
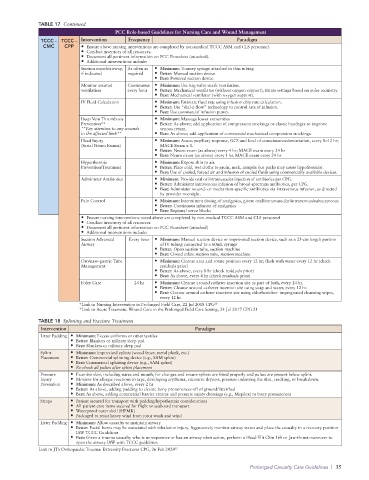
TABLE 17 Continued
PCC Role-based Guidelines for Nursing Care and Wound Management
TCCC - TCCC - Intervention Frequency Paradigm
CMC CPP • Ensure above nursing interventions are completed by non-medical TCCC ASM and CLS personnel.
• Conduct inventory of all resources.
• Document all pertinent information on PCC Flowsheet (attached).
• Additional interventions include:
Suction mouth/airway, As often as • Minimum: Toomey syringe attached to thin tubing
if indicated required • Better: Manual suction device
• Best: Powered suction device
Monitor assisted Continuous: • Minimum: Use bag-valve-mask ventilation.
ventilation every hour • Better: Mechanical ventilator (without oxygen support), titrate settings based on pulse oximetry.
• Best: Mechanical ventilator (with oxygen support).
IV Fluid Calculation • Minimum: Estimate fluid rate using infusion drip rate calculation.
• Better: Use “dial-a-flow” technology to control rate of infusion.
• Best: Use commercial infusion pump.
Deep Vein Thrombosis • Minimum: Massage lower extremities
Prevention** • Better: As above; add application of compression stockings or elastic bandages to improve
**Pay attention to any wounds venous return.
to the affected limb** • Best: As above; add application of commercial mechanical compression stockings.
Head Injury • Minimum: Assess pupillary response, GCS and level of consciousness/orientation, every 8–12 hr;
(Serial Neuro Exams) MACE Exam x 1.
• Better: Neuro exam (as above) every 4 hr; MACE exam every 24 hr
• Best: Neuro exam (as above) every 1 hr, MACE exam every 24 hr
Hyperthermia • Minimum: Expose skin to air.
Prevention/Treatment • Better: Place cold, wet cloths to groin, neck, armpits (ice packs may cause hypothermia).
• Best: Use of cooled, forced air and infusion of cooled fluids using commercially available devices.
Administer Antibiotics • Minimum: Provide oral or intramuscular injection of antibiotics per CPG.
• Better: Administer intravenous infusion of broad-spectrum antibiotics, per CPG.
• Best: Administer wound- or mechanism-specific antibiotics via intravenous infusion, as directed
by provider oversight.
Pain Control • Minimum: Intermittent dosing of analgesics, given: oral/intramuscular/intravenous/subcutaneous
• Better: Continuous infusion of analgesics
• Best: Regional nerve blocks
• Ensure nursing interventions noted above are completed by non-medical TCCC ASM and CLS personnel
• Conduct inventory of all resources
• Document all pertinent information on PCC Flowsheet (attached)
• Additional interventions include:
Suction Advanced Every hour • Minimum: Manual suction device or improvised suction device, such as a 25-cm length portion
Airway of IV tubing connected to a 60mL syringe
• Better: Open suction tube, suction machine
• Best: Closed inline suction tube, suction machine
Oro/naso-gastric Tube • Minimum: Cleanse area and rotate position every 12 hr; flush with water every 12 hr (check
Management residuals prior)
• Better: As above, every 8 hr (check residuals prior)
• Best: As above, every 4 hr (check residuals prior)
Foley Care 24 hr • Minimum: Cleanse around catheter insertion site as part of bath, every 24 hr.
• Better: Cleanse around catheter insertion site using soap and water, every 12 hr.
• Best: Cleanse around catheter insertion site using chlorhexidine- impregnated cleansing wipes,
every 12 hr.
*Link to Nursing Intervention in Prolonged Field Care, 22 Jul 2018 CPG 20
*Link to Acute Traumatic Wound Care in the Prolonged Field Care Setting, 24 Jul 2017 CPG 21
TABLE 18 Splinting and Fracture Treatment
Intervention Paradigm
Litter Padding • Minimum: Excess uniforms or other textiles
• Better: Blankets or military sleep pad
• Best: Blankets or military sleep pad
Splint • Minimum: Improvised splints (wood fence, metal plank, etc.)
Placement • Better: Commercial splinting device (e.g., SAM splint)
• Best: Commercial splinting device (e.g., SAM splint)
• Re-check all pulses after splint placement
Pressure • Examine skin, including nares and mouth, for changes and ensure splints are fitted properly and pulses are present below splint.
Injury • Monitor for allergic reactions to tape, developing erythema, excessive dryness, pressure indenting the skin, cracking, or breakdown.
Prevention • Minimum: As described above, every 2 hr
• Better: As above, adding padding to elevate bony prominences off of ground/litter/bed
• Best: As above, adding commercial barrier creams and pressure injury dressings (e.g., Mepilex) to bony prominences
Straps • Patient secured for transport with padding/hypothermia considerations
• All patient care items secured for flight or seaboard transport
• Waterproof outer shell (HPMK)
• Packaged to resist heavy wind from rotor wash and wind
Litter Padding • Minimum: Allow casualty to maintain airway
• Better: Facial burns may be associated with inhalation injury. Aggressively monitor airway status and place the casualty in a recovery position
IAW TCCC Guidelines
• Best: Given a trauma casualty who is unresponsive or has an airway obstruction, perform a Head-Tilt Chin Lift or Jaw-thrust maneuver to
open the airway IAW with TCCC guidelines
Link to JTS Orthopaedic Trauma: Extremity Fractures CPG, 26 Feb 2020 22
Prolonged Casualty Care Guidelines | 35