Page 50 - 2020 JSOM Winter
P. 50
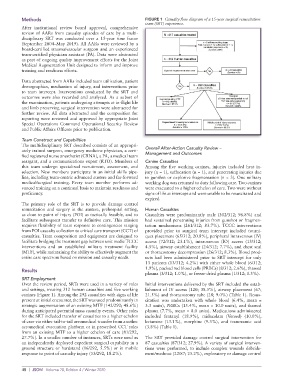
Methods FIGURE 1 Casualty flow diagram of a 15-year surgical resuscitation
team (SRT) experience.
After institutional review board approval, comprehensive
review of AARs from casualty episodes of care by a multi-
disciplinary SRT was conducted over a 15-year time frame
(September 2004–May 2019). All AARs were reviewed by a
board-certified trauma/vascular surgeon and an experienced
team-certified physician assistant (PA). Data were abstracted
as part of ongoing quality improvement efforts for the Joint
Medical Augmentation Unit designed to inform and improve
training and readiness efforts.
Data abstracted from AARs included team utilization, patient
demographics, mechanism of injury, and interventions prior
to team intercept. Interventions conducted by the SRT and
outcomes were also recorded and analyzed. As a subset of
the examination, patients undergoing attempts at in-flight life
and limb preserving surgical intervention were abstracted for
further review. All data abstracted and the composition for
reporting were reviewed and approved by appropriate Joint
Special Operations Command Operational Security Review
and Public Affairs Officers prior to publication.
Team Construct and Capabilities
The multidisciplinary SRT described consists of an appropri-
ately trained surgeon, emergency medicine physician, a certi- Overall After-Action Casualty Review –
fied registered nurse anesthetist (CRNA), a PA, a medical team Management and Outcomes
seargant, and a communications expert (RTO). Members of Canine Casualties
this team undergo specialized recruitment, assessment, and Among the five working canines, injuries included heat in-
selection. New members participate in an initial skills pipe- jury (n = 1), suffocation (n = 1), and penetrating injuries due
line, including team-centric advanced austere and far-forward to gunshot or explosive fragmentation (n = 3). One military
medical/surgical training. Every team member performs ad- working dog was returned to duty following care. Two canines
vanced training on a continual basis to maintain readiness and were evacuated to a higher echelon of care. Two were without
proficiency. signs of life at intercept and were unable to be resuscitated and
expired.
The primary role of the SRT is to provide damage control
resuscitation and surgery in the austere, prehospital setting, Human Casualties
as close to point of injury (POI) as tactically feasible, and to Casualties were predominantly male (302/312; 96.8%) and
facilitate subsequent transfer to definitive care. This mission had sustained penetrating injuries from gunshot or fragmen-
requires flexibility of team response to contingencies ranging tation mechanisms (261/312; 83.7%). TCCC interventions
from POI casualty collection to critical care transport (CCT) of provided prior to surgical team intercept included tourni-
casualties. Team composition and equipment are designed to quet placement (65/312; 20.8%), peripheral intravenous (IV)
facilitate bridging the treatment gap between unit medic TCCC access (72/312; 23.1%), intraosseous (IO) access (13/312;
interventions and an established military treatment facility 4.5%), airway establishment (24/312; 7.7%), and chest seal
(MTF), while maintaining the ability to effectively augment the or thoracostomy decompression (26/312; 8.3%). Blood prod-
entire care spectrum based on mission and casualty needs. ucts had been administered prior to SRT intercept for only
13 patients (13/312; 4.2%) with either whole blood (6/312;
Results 1.9%), packed red blood cells (PRBCs) (8/312; 2.6%), thawed
plasma (3/312; 1.0%), or freeze-dried plasma (1/312; 0.3%).
SRT Employment
Over the review period, SRTs were used in a variety of roles Initial interventions delivered by the SRT included the estab-
and settings, treating 312 human casualties and five working lishment of IV access (120; 38.5%), airway placement (67;
canines (Figure 1). Among the 292 casualties with signs of life 21.5%) and thoracostomy tube (28; 9.0%) (Table 1). Resus-
present at initial encounter, the SRT was used predominantly in citation was undertaken with whole blood (6.4%, mean =
strategic augmentation of an existing MTF (142/292; 48.6%) 3.3 units), PRBCs (15.4%, mean = 10.0 units), and thawed
during anticipated potential mass casualty events. Other roles plasma (7.7%, mean = 8.0 units). Medications administered
for the SRT included transfer of casualties to a higher echelon included fentanyl (18.9%), midazolam (Versed) (10.0%),
of care via either tail-to-tail aeromedical transfer from another ketamine (13.1%), morphine (9.3%), and tranexamic acid
aeromedical evacuation platform or in prescribed CCT roles (3.8%) (Table 1).
from an existing MTF to a higher echelon of care (81/292,
27.7%). In a smaller number of instances, SRTs were used as The SRT provided damage control surgical intervention for
an independently deployed expedient surgical capability in a 87 casualties (87/312; 27.9%). A variety of surgical interven-
ground structure or hardstand (16/292, 5.5%) or in mobile tions were performed, to include complex wounds debride-
response to point of casualty injury (53/292, 18.2%). ment/washout (22/87; 25.2%), exploratory or damage control
48 | JSOM Volume 20, Edition 4 / Winter 2020