Page 51 - 2020 JSOM Winter
P. 51
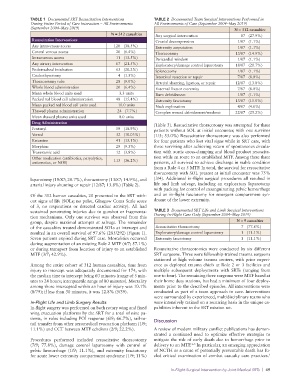
TABLE 1 Documented SRT Resuscitation Interventions TABLE 2 Documented Team Surgical Interventions Performed in
During Entire Period of Care Interaction – All Environments All Environments of Care (September 2004–May 2019)
(September 2004–May 2019) N = 312 casualties
N = 312 casualties Any surgical intervention 87 (27.9%)
Resuscitation Interventions Cranial decompression 1/87 (1.1%)
Any intravenous access 120 (38.5%) Extremity amputation 1/87 (1.1%)
Central venous access 20 (6.4%) Thoracotomy 13/87 (14.9%)
Intraosseous access 11 (13.5%) Pericardial window 1/87 (1.1%)
Any airway intervention 67 (21.5%) Exploratory/damage control laparotomy 18/87 (20.7%)
Endotracheal intubation 63 (20.2%) Splenectomy 1/87 (1.1%)
Crichothyrotomy 4 (1.3%) Intestinal resection or repair 7/87 (8.0%)
Thoracostomy tube 28 (9.0%) Arterial shunting, ligation, or repair 12/87 (13.8%)
Whole blood administration 20 (6.4%) External fixator extremity 7/87 (8.0%)
Mean whole blood units used 3.3 units Burn debridement 1/87 (1.1%)
Packed red blood cell administration 48 (15.4%) Extremity fasciotomy 13/87 (15.0%)
Mean packed red blood cell units used 10.0 units Neck exploration 4/87 (4.6%)
Thawed plasma administration 24 (7.7%) Complex wound debridement/washout 22/87 (25.2%)
Mean thawed plasma units used 8.0 units
Drug Administration (Table 3). Resuscitative thoracotomy was attempted for three
Fentanyl 59 (18.9%) patients without SOL at initial encounter, with one survivor
Versed 32 (10.03%) (1/3; 33.0%) Resuscitative thoracotomy was also performed
Ketamine 41 (13.1%) for four patients who lost vital signs while in SRT care, with
Morphine 29 (9.3%) three surviving after achieving return of spontaneous circula-
Tranexamic acid 12 (3.8%) tion with aortic cross-clamping and blood product resuscita-
Other medication (antibiotics, paryalytics, 113 (36.2%) tion while en route to an established MTF. Among these three
antiemetics, or NOS) patients, all survived to achieve discharge in stable condition
from a Role 4 or 5 MTF. In total, the survival for resuscitative
thoracotomy with SOL present at initial encounter was 75%
laparotomy (18/87; 20.7%), thoracotomy (13/87; 14.9%), and (3/4). Additional in-flight surgical procedures all resulted in
arterial injury shunting or repair (12/87; 13.8%) (Table 2). life and limb salvage, including an exploratory laparotomy
with packing for control of exsanguinating pelvic hemorrhage
Of the 312 human casualties, 20 presented to the SRT with- and an in-flight fasciotomy for emergent compartment syn-
out signs of life (SOLs; no pulse, Glasgow Coma Scale score drome of the lower extremity.
of 3, no respirations or detected cardiac activity). All had
sustained penetrating injuries due to gunshot or fragmenta- TABLE 3 Documented SRT Life and Limb Surgical Interventions
tion mechanisms. Only one survivor was observed from this During In-Flight Care Only (September 2004–May 2019)
group, despite maximal attempts at salvage. The remainder N = 9 casualties
of the casualties treated demonstrated SOLs at intercept and Resuscitative thoracotomy 7 (77.8%)
resulted in an overall survival of 97.6% (285/292) (Figure 1). Exploratory/damage control laparotomy 1 (11.1%)
Seven patients expired during SRT care. Mortalities occurred Extremity fasciotomy 1 (11.1%)
during augmentation of an existing Role 2 MTF (4/7; 57.1%)
or during transport from location of injury to an established Resuscitative thoracotomies were conducted by six different
MTF (3/7; 42.9%). SRT surgeons. Three were fellowship-trained trauma surgeons
stationed at high volume trauma centers, with prior experi-
Among the entire cohort of 312 human casualties, time from ence as deployed trauma chiefs at Role 2 or 3 facilities and
injury to intercept was adequately documented for 174, with multiple subsequent deployments with SRTs (ranging from
the median time to intercept being 60 minutes (range of 5 min- one to four). The remaining three surgeons were MTF based at
utes to 24 hours; interquartile range of 80 minutes). Mortality their home duty stations, but had a minimum of four deploy-
among those intercepted within an hour of injury was 10.1% ments prior to the described episodes. All interventions were
(8/79); if less than 30 minutes, it was 12.8% (5/39). conducted as part of a team approach to care. Interventions
were surrounded by experienced, multidisciplinary teams who
In-Flight Life and Limb Surgery Results were intensively trained on a recurring basis in the unique ca-
In-flight surgery was performed on both rotary wing and fixed pabilities inherent to the SRT mission set.
wing evacuation platforms by the SRT for a total of nine pa-
tients, in roles including POI response (6/9; 66.7%), tail-to- Discussion
tail transfer from other aeromedical evacuation platform (1/9;
11.1%) and CCT between MTF echelons (2/9; 22.2%). A review of modern military conflict publications has demon-
strated a continued need to optimize effective strategies to
Procedures performed included resuscitative thoracotomy mitigate the risk of early death due to hemorrhage prior to
(7/9; 77.8%), damage control laparotomy with control of delivery to an MTF. In particular, an emerging appreciation
1–5
pelvic hemorrhage (1/9; 11.1%), and extremity fasciotomy of NCTH as a cause of potentially preventable death has fu-
for acute lower extremity compartment syndrome (1/9; 11%) eled critical examination of combat casualty care practices.
1
In-Flight Surgical Intervention by Joint Medical SRTs | 49