Page 110 - JSOM Fall 2019
P. 110
Infection occurs most commonly in the creases and folds of permethrin treatment fails, oral ivermectin (200 μg/kg) may be
the body: the space between the fingers, the armpits, the inter- given in two doses, also 1 week apart, to kill the scabies mites.
gluteal cleft and the navel. In young children the rash may be For patients with crusted scabies, daily combination therapy
more widespread and present on the scalp, face, neck, palms, with permethrin cream and oral ivermectin for at least 1 week
and soles. Immunocompromised, malnourished or chronic is often required. Lindane should not be used due to concern
corticosteroid users are more likely to develop crusted scabies for adverse effects, including seizures.
with malodorous, crusty scales on a reddened base. Occasion-
ally the only indications of infection are scattered small, red- In order to kill the mites and prevent recontamination, all
brown papules in the genital region (Figure 3). clothing and bedding should be washed in hot water and dried
on high heat in conjunction with treatment. If it is not possible
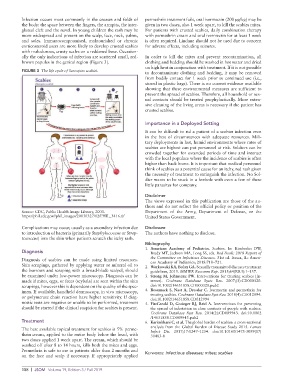
FIGURE 3 The life cycle of Sarcoptes scabiei.
to decontaminate clothing and bedding, it may be removed
from bodily contact for 1 week prior to continued use (i.e.,
stored in plastic bags). There is no current evidence available
showing that these environmental measures are sufficient to
prevent the spread of scabies. Therefore, all household or sex-
ual contacts should be treated prophylactically. More exten-
sive cleaning of the living areas is necessary if the patient has
crusted scabies.
Importance in a Deployed Setting
It can be difficult to rid a patient of a scabies infection even
in the best of circumstances with adequate resources. Mili-
tary deployments in hot, humid environments where rates of
scabies are highest can put personnel at risk. Soldiers can be
crowded together for extended periods of time and interact
with the local populace where the incidence of scabies is often
higher than back home. It is important that medical personnel
think of scabies as a potential cause for an itchy, red rash given
the necessity of treatment to extinguish the infection. No Sol-
dier wants to be stuck in a foxhole with even a few of these
little parasites for company.
Disclaimer
The views expressed in this publication are those of the au-
thors and do not reflect the official policy or position of the
Source: CDC, Public Health Image Library, 2003. Department of the Army, Department of Defense, or the
https://phil.cdc.gov//phil_images/20030327/12/PHIL_3416.tif United States Government.
Complications may occur, usually as a secondary infection due Disclosure
to introduction of bacteria (primarily Staphylococcus or Strep- The authors have nothing to disclose.
tococcus) into the skin when patients scratch the itchy rash.
Bibliography
1. American Academy of Pediatrics. Scabies. In: Kimberlin DW,
Diagnosis Brady MT, Jackson MA, Long SS, eds. Red Book: 2018 Report of
Diagnosis of scabies can be made using limited resources. the Committee on Infectious Diseases. 31st ed. Itasca, IL: Ameri-
can Academy of Pediatrics; 2018:718–721.
Skin scrapings, gathered by applying water or mineral oil to 2. Workowski KA, Bolan GA. Sexually transmitted diseases treatment
the burrows and scraping with a broad-blade scalpel, should guidelines, 2015. MMWR Recomm Rep. 2015;64(RR3):1–137.
be examined under low-power microscopy. Diagnosis can be 3. Strong M, Johnstone PW. Interventions for treating scabies [In-
made if mites, eggs, or feces (scybala) are seen within the skin ternet]. Cochrane Database Systc Rev. 2007;(3):CD000320.
scrapings, however this is dependent on the quality of the spec- doi:10.1002/14651858.CD000320.pub2
imen. If available, handheld dermoscopy, in vivo microscopy, 4. Rosumeck S, Nast A, Dressler C. Ivermectin and permethrin for
or polymerase chain reaction have higher sensitivity. If diag- treating scabies. Cochrane Database Syst Rev. 2018(4):CD012994.
doi:10.1002/14651858.CD012994
nostic tests are negative or unable to be performed, treatment 5. FitzGerald D, Grainger RJ, Reid A. Interventions for preventing
should be started if the clinical suspicion for scabies is present. the spread of infestation in close contacts of people with scabies.
Cochrane Database Syst Rev. 2014(2):CD009943. doi:10.1002
/14651858.CD009943.pub2
Treatment 6. Karimkhani C, et al. The global burden of scabies: a cross- sectional
The best available topical treatment for scabies is 5% perme- analysis from the Global Burden of Disease Study 2015. Lancet
thrin cream, applied to the entire body below the head, with Infect Dis. 2017;17:1247–1254. doi:10.1016/S1473-3099(17)
30483-8
two doses applied 1 week apart. The cream, which should be
washed off after 8 to 14 hours, kills both the mites and eggs.
Permethrin is safe to use in patients older than 2 months and
on the face and scalp if necessary. If appropriately applied Keywords: infectious diseases; mites; scabies
108 | JSOM Volume 19, Edition 3 / Fall 2019