Page 50 - JSOM Fall 2020
P. 50
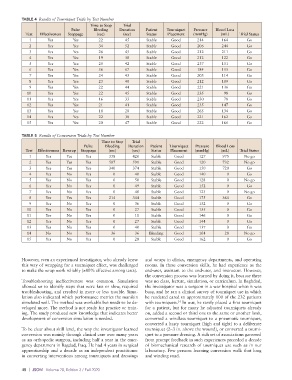
TABLE 4 Results of Tourniquet Trials by Test Number
Time to Stop Trial
Pulse Bleeding Duration Patient Tourniquet Pressure Blood Loss
Test Effectiveness Stoppage (sec) (sec) Status Placement (mmHg) (mL) Trial Status
1 Yes Yes 22 45 Stable Good 214 164 Go
2 Yes Yes 34 52 Stable Good 206 244 Go
3 Yes Yes 26 45 Stable Good 212 211 Go
4 Yes Yes 19 38 Stable Good 212 122 Go
5 Yes Yes 25 42 Stable Good 237 151 Go
6 Yes Yes 56 67 Stable Good 184 155 Go
7 Yes Yes 24 43 Stable Good 203 114 Go
8 Yes Yes 23 40 Stable Good 212 109 Go
9 Yes Yes 22 44 Stable Good 221 136 Go
10 Yes Yes 22 45 Stable Good 235 98 Go
11 Yes Yes 16 33 Stable Good 230 78 Go
12 Yes Yes 21 41 Stable Good 235 147 Go
13 Yes Yes 18 28 Stable Good 265 134 Go
14 Yes Yes 22 38 Stable Good 221 162 Go
15 Yes Yes 20 47 Stable Good 222 166 Go
TABLE 5 Results of Conversion Trials by Test Number
Time to Stop Trial
Pulse Bleeding Duration Patient Tourniquet Pressure Blood Loss
Test Effectiveness Rewrap Stoppage (sec) (sec) Status Placement (mmHg) (mL) Trial Status
1 Yes Yes Yes 338 420 Stable Good 127 975 No go
2 Yes Yes Yes 507 591 Stable Good 120 732 No go
3 Yes Yes Yes 340 374 Stable Good 150 720 Go
4 Yes No Yes 0 40 Stable Good 140 0 Go
5 Yes No Yes 0 50 Stable Good 128 0 No go
6 Yes No Yes 0 49 Stable Good 152 0 Go
7 Yes No Yes 0 40 Stable Good 123 0 No go
8 Yes Yes Yes 214 344 Stable Good 175 364 Go
9 Yes No Yes 0 36 Stable Good 152 0 Go
10 Yes No Yes 0 27 Stable Good 155 0 Go
11 Yes No Yes 0 11 Stable Good 146 0 Go
12 Yes No Yes 0 27 Stable Good 144 0 Go
13 Yes No Yes 0 40 Stable Good 137 0 Go
14 No No Yes 36 36 Bleeding Good 104 28 No go
15 Yes No Yes 0 28 Stable Good 162 0 Go
However, even an experienced investigator, who already knew and wraps in clinics, emergency departments, and operating
this way of wrapping for a tourniquet effect, was challenged rooms. In these conversion skills, he had experience as the
to make the wrap work reliably (≥80% effective among tests). end-user, assistant to the end-user, and instructor. However,
the conversion process was learned by doing it, because there
Troubleshooting ineffectiveness was common. Simulation was no class, lecture, simulation, or curriculum. In Baghdad,
allowed us to identify steps that were fast or slow, required the investigator was a surgeon in a war hospital when it was
troubleshooting, and resulted in more or less trouble. Simu- busy, and he ran a clinical survey of tourniquet use in which
lation also indicated which performance metrics the manikin he rendered cared to approximately 100 of the 232 patients
simulated well. The method was workable but needs to be de- with tourniquets. In war, he rarely placed a first tourniquet
14
veloped more. The method is not ready for practice or train- for a patient, but for many he adjusted tourniquets already
ing. The study produced new knowledge that indicates better on, added a second or third one to the same or another limb,
development of conversion simulation is needed. converted a windlass tourniquet to a pneumatic tourniquet,
converted a hasty tourniquet (high and tight) to a deliberate
To be clear about skill level, the way the investigator learned tourniquet (2–3 in. above the wound), or converted a tourni-
conversion was mainly through clinical care over many years quet to a pressure dressing. A rich set of associations garnered
as an orthopedic surgeon, including half a year in the emer- from prompt feedback in such experiences preceded a decade
gency department in Bagdad, Iraq. He had 4 years in surgical of biomechanical research of tourniquet use such as in our
apprenticeship and a decade as an independent practitioner laboratory. Few persons learning conversion walk that long
in converting interventions among tourniquets and dressings and winding road.
48 | JSOM Volume 20, Edition 3 / Fall 2020