Page 157 - JSOM Fall 2020
P. 157
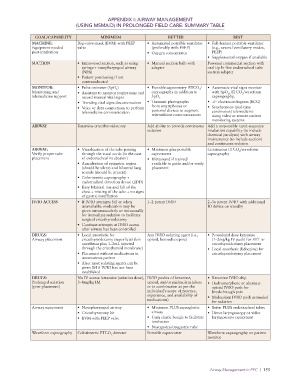
APPENDIX I: AIRWAY MANAGEMENT
(USING MSMAID) IN PROLONGED FIELD CARE: SUMMARY TABLE
GOAL/CAPABILITY MINIMUM BETTER BEST
MACHINE: Bag-valve-mask (BVM) with PEEP • Automated portable ventilator • Full-feature portable ventilator
Equipment needed valve (preferably with PEEP) (e.g., several ventilatory modes,
post-intubation • Oxygen concentrator PEEP)
• Supplemental oxygen if available
SUCTION • Improvised suction, such as using • Manual suction bulb with Powered commercial suction with
syringe + nasopharyngeal airway adapter oral tip In-line endotracheal tube
(NPA) suction adapter
• Patient positioning if not
contraindicated
MONITOR: • Pulse oximeter (SpO ) • Portable capnometry ETCO / • Automatic vital signs monitor
2
2
Monitoring and • Assistant to monitor respirations and capnography in addition to with SpO , ETCO /waveform
2
2
telemedicine support record manual vital signs SpO 2 capnography,
• Trending vital signs documentation • Transmit photographs • +/– electrocardiogram (ECG)
• Voice or data connections to perform from smartphones or • Synchronous (real-time
telemedicine communication personal devices to augment continuous) telemedicine
telemedicine communications using video or remote patient
monitoring systems
AIRWAY Ketamine cricothyroidotomy Add ability to provide continuous Add a responsible rapid-sequence
sedation intubation capability (to include
chemical paralysis) with airway
maintenance (to include suction)
and continuous sedation
AIRWAY: • Visualization of the tube passing • Minimum plus portable Continuous ETCO /waveform
2
Verify proper tube through the vocal cords (in the case capnometer capnography
placement of endotracheal intubation) • Ultrasound if trained/
• Auscultation of epigastric region available to guide and/or verify
(should be silent) and bilateral lung placement
sounds (should be present)
• Colorimetric capnography +
endotracheal detection device (EDD)
• Easy bilateral rise and fall of the
chest + misting of the tube + no signs
of gastric insufflation
IV/IO ACCESS • If IV/IO attempts fail or when 1–2 patent IV/IO 2–3× patent IV/IO with additional
unavailable: medication may be IO device on standby
given intramuscularly or intranasally
for immediate sedation to facilitate
surgical cricothyroidotomy
• Continue attempts at IV/IO access
after airway has been controlled
DRUGS: • Local anesthetic for Any IV/IO sedating agent (i.e., • Procedural dose ketamine
Airway placement cricothyroidotomy (superficial skin opioid, benzodiazepine) (1–2mg/kg IV push) for ETT or
anesthesia plus 1–2mL injected cricothyroidotomy placement
through the cricothyroid membrane) • Local anesthetic (lidocaine) for
• Placement without medications in cricothyroidotomy placement
unconscious patient
• Also: most sedating agents can be
given IM if IV/IO has not been
established
DRUGS: No IV access: ketamine (sedation dose), IV/IO pushes of ketamine, • Ketamine IV/IO drip
Prolonged sedation 3–4mg/kg IM opioid, and/or midazolam (alone • Hydromorphone or alternate
(post-placement) or in combination as per the opioid IV/IO push for
individual’s scope of practice, breakthrough pain
experience, and availability of • Midazolam IV/IO push as needed
medications) for sedation
Airway equipment • Nasopharyngeal airway • Minimum PLUS supraglottic • Better PLUS endotracheal tubes
• Cricothyrotomy kit airway • Direct laryngoscopy or video
• BVM with PEEP valve • Gum elastic bougie to facilitate laryngoscopy equipment
intubation
• Nasogastric/orogastric tube
Waveform capnography Colorimetric ETCO detector Portable capnometer Waveform capnography on patient
2
monitor
Airway Management in PFC | 155