Page 84 - Journal of Special Operations Medicine - Fall 2016
P. 84
renal tubular obstructions (pigmented “casts”). Organic Figure 1 Incidence of exertional rhabdomyolysis in the
acids released from the myocytes can cause metabolic military, 2004–2015. Cases were compiled using ICD-9 codes
acidosis. ER can occur in individuals performing fa- 728.88 (rhabdomyolysis) and/or 791.3 (myoglobinuria), plus
1–3
miliar physical activity, but in these cases, the medical a diagnosis of one of the following: 276.50–276.52 (volume
provider should suspect an underlying infection or the depletion/dehydration), 992.0–992.9 (effects of heat), 994.3
(effects of thirst/deprivation of water), or 994.4–994.5
use of a new medication or dietary supplement. (exhaustion due to exposure or excessive exertion). 35–43
There are numerous case reports of ER in the literature
associated with military training, 4–11 but also cases dur-
ing police recruit training, 12,13 in testing of firefighter
candidates, among prison inmates, in school chil-
14
12
dren, and even cases involving personal trainers.
16
15
Virtually any type of physical activity performed in
excess to what the individual is accustomed can pre-
cipitate ER. Cases have been reported in swim train-
ing, bodybuilding and weight lifting, 18–21 callisthenic
17
exercises, 22–24 snowboarding, stationary cycling, 26,27
25
football training, 24,28,29 gardening, and during extreme
30
exercise programs. 31,34 Outbreaks involving multiple in-
dividuals participating in exercise have occurred in the
military, 6,9,11 but also in police, athletic training, 17,24,29
12
and high school physical education. Rhabdomyolysis
15
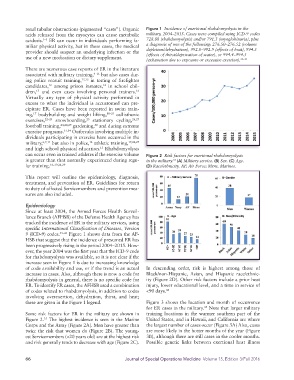
can occur even in trained athletes if the exercise volume Figure 2 Risk factors for exertional rhabdomyolysis
is greater than that normally experienced during regu- in the military. (A) Military service. (B) Sex. (C) Age.
35
lar training. 16–19,24,29 (D) Race/ethnicity. AF, Air Force; Mrns, Marines.
This report will outline the epidemiology, diagnosis,
treatment, and prevention of ER. Guidelines for return
to duty of affected Servicemembers and prevention mea-
sures are also included.
Epidemiology
Since at least 2004, the Armed Forces Health Surveil-
lance Branch (AFHSB) of the Defense Health Agency has
tracked the incidence of ER in the military services, using
specific International Classification of Diseases, Version
9 (ICD-9) codes. 35–43 Figure 1 shows data from the AF-
HSB that suggest that the incidence of presumed ER has
been progressively rising in the period 2004–2015. How-
ever, the year 2004 was the first year that the ICD-9 code
for rhabdomyolysis was available, so it is not clear if the
increase seen in Figure 1 is due to increasing knowledge
of code availability and use, or if the trend is an actual In descending order, risk is highest among those of
increase in cases. Also, although there is now a code for Black/non-Hispanic, Asian, and Hispanic race/ethnic-
rhabdomyolysis in general, there is no specific code for ity (Figure 2D). Other risk factors include a prior heat
ER. To identify ER cases, the AFHSB used a combination injury, lower educational level, and a time in service of
of codes related to rhabdomyolysis, in addition to codes <90 days. 44
involving overexertion, dehydration, thirst, and heat;
these are given in the Figure 1 legend. Figure 3 shows the location and month of occurrence
for ER cases in the military. Note that larger military
35
Some risk factors for ER in the military are shown in training locations in the warmer southern part of the
Figure 2. The highest incidence is seen in the Marine United States, and in Hawaii, and California are where
35
Corps and the Army (Figure 2A). Men have greater than the largest number of cases occur (Figure 3A) Also, cases
twice the risk that women do (Figure 2B). The young- are more likely in the hotter months of the year (Figure
est Servicemembers (<20 years old) are at the highest risk 3B), although there are still cases in the cooler months.
and risk generally tends to decrease with age (Figure 2C). Possible genetic links between exertional heat illness
66 Journal of Special Operations Medicine Volume 15, Edition 3/Fall 2016