Page 41 - PJ MED OPS Handbook 8th Ed
P. 41
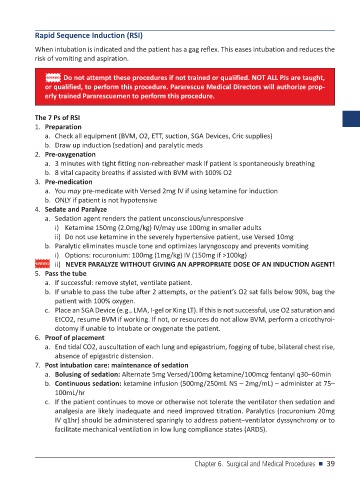
Rapid Sequence Induction (RSI)
When intubation is indicated and the patient has a gag reflex. This eases intubation and reduces the
risk of vomiting and aspiration.
WARNING Do not attempt these procedures if not trained or qualified. NOT ALL PJs are taught,
or qualified, to perform this procedure. Pararescue Medical Directors will authorize prop-
erly trained Pararescuemen to perform this procedure.
The 7 Ps of RSI
1. Preparation
a. Check all equipment (BVM, O2, ETT, suction, SGA Devices, Cric supplies)
b. Draw up induction (sedation) and paralytic meds
2. Pre-oxygenation
a. 3 minutes with tight fitting non-rebreather mask if patient is spontaneously breathing
b. 8 vital capacity breaths if assisted with BVM with 100% O2
3. Pre-medication
a. You may pre-medicate with Versed 2mg IV if using ketamine for induction
b. ONLY if patient is not hypotensive
4. Sedate and Paralyze
a. Sedation agent renders the patient unconscious/unresponsive
i) Ketamine 150mg (2.0mg/kg) IV/may use 100mg in smaller adults
ii) Do not use ketamine in the severely hypertensive patient, use Versed 10mg
b. Paralytic eliminates muscle tone and optimizes laryngoscopy and prevents vomiting
i) Options: rocuronium: 100mg (1mg/kg) IV (150mg if >100kg)
ii) NEVER PARALYZE WITHOUT GIVING AN APPROPRIATE DOSE OF AN INDUCTION AGENT!
5. Pass the tube
a. If successful: remove stylet, ventilate patient.
b. If unable to pass the tube after 2 attempts, or the patient’s O2 sat falls below 90%, bag the
patient with 100% oxygen.
c. Place an SGA Device (e.g., LMA, I-gel or King LT). If this is not successful, use O2 saturation and
EtCO2, resume BVM if working. If not, or resources do not allow BVM, perform a cricothyroi-
dotomy if unable to intubate or oxygenate the patient.
6. Proof of placement
a. End tidal CO2, auscultation of each lung and epigastrium, fogging of tube, bilateral chest rise,
absence of epigastric distension.
7. Post intubation care: maintenance of sedation
a. Bolusing of sedation: Alternate 5mg Versed/100mg ketamine/100mcg fentanyl q30–60min
b. Continuous sedation: ketamine infusion (500mg/250mL NS – 2mg/mL) – administer at 75–
100mL/hr
c. If the patient continues to move or otherwise not tolerate the ventilator then sedation and
analgesia are likely inadequate and need improved titration. Paralytics (rocuronium 20mg
IV q1hr) should be administered sparingly to address patient–ventilator dyssynchrony or to
facilitate mechanical ventilation in low lung compliance states (ARDS).
Chapter 6. Surgical and Medical Procedures n 39