Page 124 - 2020 JSOM Winter
P. 124
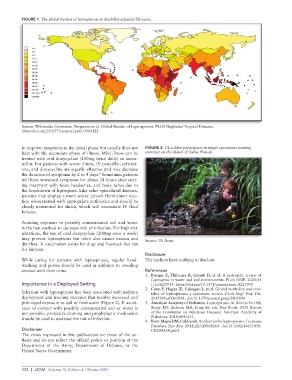
FIGURE 1 The global burden of leptospirosis in disability-adjusted life-years.
Source: Wikimedia Commons. Torgerson et al. Global Burden of Leptospirosis. PLOS Neglected Tropical Diseases.
https://doi.org/10.1371/journal.pntd.0004122
to improve symptoms in the initial phase but usually does not FIGURE 2 US soldier participates in jungle operations training
help with the secondary phase of illness. Mild illness can be exercises on the island of Oahu, Hawaii.
treated with oral doxycycline (100mg twice daily) or amox-
icillin. For patients with severe illness, IV penicillin, ceftriax-
one, and doxycycline are equally effective and may decrease
4
the duration of symptoms by 2 to 4 days. Sometimes patients
will have worsened symptoms for about 24 hours after start-
ing treatment with fever, headaches, and body aches due to
the breakdown of leptospires. Like other spirochetal diseases,
patients may display a more severe Jarisch-Herxheimer reac-
tion when treated with appropriate antibiotics and should be
closely monitored for shock, which will necessitate IV fluid
boluses.
Avoiding exposure to possibly contaminated soil and water
is the best method to decrease risk of infection. For high-risk
situations, the use of oral doxycycline (200mg once a week)
may prevent leptospirosis but often also causes nausea and Source: US Army
diarrhea. A vaccination exists for dogs and livestock but not
for humans.
Disclosure
While caring for patients with leptospirosis, regular hand- The authors have nothing to disclose.
washing and gloves should be used in addition to avoiding
contact with their urine. References
1. Bierque E, Thibeaux R, Girault D, et al. A systematic review of
Leptospira in water and soil environments. PLoS ONE. 2020;15
Importance in a Deployed Setting (1):e0227055. https://doi.org/10.1371/journal.pone.0227055
2. Costa F, Hagan JE, Calcagno J, et al. Global morbidity and mor-
Infection with leptospirosis has been associated with military tality of leptospirosis: a systematic review. PLoS Negl Trop Dis.
deployment and training exercises that involve increased and 20159(9):e0003898. doi:10.1371/journal.pntd.0003898
prolonged exposure to soil or freshwater (Figure 2). If avoid- 3. American Academy of Pediatrics. Leptospirosis. In: Kimberlin DW,
ance of contact with possibly contaminated soil or water is Brady MT, Jackson MA, Long SS, eds. Red Book: 2018 Report
not possible, protective clothing and prophylactic medication of the Committee on Infectious Diseases. American Academy of
should be used to decrease the risk of infection. Pediatrics. 2018;508–511.
4. Brett-Major DM, Coldren R. Antibiotics for leptospirosis. Cochrane
Database Syst Rev. 2012;(2):CD008264. doi:10.1002/14651858.
Disclaimer CD008264.pub2
The views expressed in this publication are those of the au-
thors and do not reflect the official policy or position of the
Department of the Army, Department of Defense, or the
United States Government.
122 | JSOM Volume 20, Edition 4 / Winter 2020