Page 132 - JSOM Fall 2020
P. 132
➝ CO, lung edema compared to ➝ CO, brain injury markers, stress- acid-
hypotensive resuscitation fluid. ALM is a potent ALM correction indicates clotting factors present & pathways operational. ALM possible anti- fibrinolytic. 27,46,47 resection. ALM ➝ Hextend led to poor outcomes. 31 3% NaCl ALM led to 100% 3-day survival with and brain and downregulated periphery. 33 0.9% NaCl ALM induced a reversible hypotensive, antiarrhythmic state, and ➝ injury, and prevented immunosuppression. 75% mortality in co
Other Major Outcomes First report showing 7.5% NaCl ALM as a possible antiarrhythmic. Hextend led to increased mortality. 16,17 No deaths in ALM animals. 75% mortality in saline controls. ALM animals showed 89-96% reduction in Controls failed to clot at 5 and 60 min. 7.5% NaCl *3% NaCl ALM improved 6 hours survival after liver internal bleeding by 60%; ➝ flow to gut, kidney; preserved platelet aggregation. immune protection and platelet pre
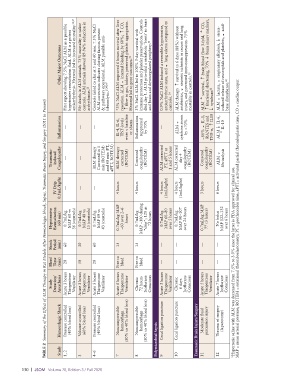
TABLE 2 Summary of the Effect of ALM Therapy in Rat Models After Hemorrhagic Shock, Sepsis, Traumatic Brain Injury, and Surgery (2011 to Present)
Inflammation — — arrhythmias. 23 — IL-4, IL-6, TNF-levels were < baseline or shams Inflammation suppressed by 70% — controls. 24 ALM therapy ALM ➝ antibiotics, ➝ cytokine storm by >70% ALM IL-1, ~80% ➝ RANTES and ➝ TNF-α, ➝ IL10 ALM ➝ IL-6, ALM ➝ ➝ IL-10
Traumatic- induced Coagulopathy — — ALM therapy Corrected in 5 min (ROTEM) and 60 min (PT, aPTT, ROTEM) ALM therapy corrected (ROTEM) Corrected coagulopathy (ROTEM) ALM corrected PT, aPTT at 1 and 5 hours ALM corrected day 4 coagulopathy (ROTEM) Corrected coagulopathy (ROTEM) ALM ➝ fibrinolysis
IV Drip 0.5mL/kg/hr — — — 4 hours 4 hours 4 hours (1mL/kg/hr) 4 hours (1mL/kg/hr) 3 hours 6 hours
Hypotensive Resuscitation (60 min) 0.7mL/kg MAP 60 vs 36 (controls) 0.7mL/kg MAP 40 vs 15 (controls) 0.7mL/kg MAP 69 vs 43 (controls) 0.7mL/kg MAP ~60 over 2–6 hours 0.7mL/kg MAP ~100 during “drip”; 120 at 72 hours 0.7mL/kg MAP 60–80 over 5 hours 0.7mL/kg MAP 90–107 over 24 hours 0.7mL/kg MAP 77 (3 hours) No bolus MAP 122–132 over 6 hours MAP = mean arterial pressure; ROTEM = rotational thromboelastomet
Shock Period (min) 60 30 60 15 15 — — — —
Bleed Time (min) 20 50 20 Free to bleed Free to bleed — — — — *Hypertonic saline with ALM was decreased from 7.5% to 3.0% since the latter is FDA approved for clinical use.
Study Duration/ Anesthesia Acute 3 hours Thiopentone Ventilator Acute 3 hours Thiopentone Ventilator Acute 3 hours Thiopentone Ventilator Acute 6 hours Thiopentone Ventilator Chronic 72 hours Isoflurane Conscious Acute 5 hours Thiopentone Ventilator Chronic 6 days Isoflurane Conscious Acute 5 hours Thiopentone Ventilator Acute 7 hours Isoflurane Conscious
Hemorrhagic Shock Pressure controlled (40% blood loss) Volume controlled (60% blood loss) Pressure controlled (40% blood loss) Noncompressible hemorrhage (30% to 40% blood loss) Noncompressible hemorrhage (30% to 40% blood loss) Cecal ligation puncture Cecal ligation puncture Traumatic Brain Injury/Surgery Moderate fluid percussion injury Trauma of surgery (laparotomy)
Study 1, 2 3 4–6 7 8 Polymicrobial Sepsis 9 10 11 12
130 | JSOM Volume 20, Edition 3 / Fall 2020