Page 101 - JSOM Fall 2020
P. 101
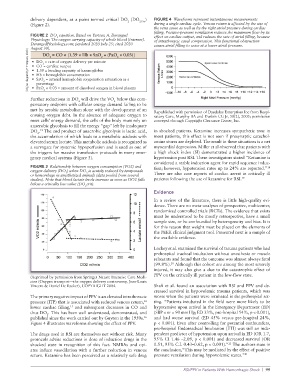
delivery dependent, at a point termed critical DO (DO 2Crit ) FIGURE 4 Waveforms represent instantaneous measurements
2
(Figure 2). during a single cardiac cycle. Venous return is affected by the size of
the vena cavae as well as by the right atrial pressure during cardiac
filling. Positive-pressure ventilation reduces the maximum flow by its
FIGURE 2 DO equation. Based on Yartsev, A. Deranged effect on cardiac output, and reduces the rate of atrial filling, because
2
Physiology: The oxygen carrying capacity of whole blood [Internet]. of intrathoracic caval compression. This functional obstruction
DerangedPhysiology.com; [updated 2020 July 25; cited 2020 causes atrial filling to cease at a lower atrial pressure.
August 30]. 2 2 2
(Original diagram by P. Thompson, 2020.) • DO = rate of oxygen delivery per minute
DO = CO × [1.39 × Hb × SaO + (PaO × 0.03)]
2
• CO = cardiac output
• 1.39 = binding capacity of haemoglobin
• Hb = hemoglobin concentration
• SaO = arterial hemoglobin oxygenation saturation as a
2
percentage
• PaO × 0.03 = amount of dissolved oxygen in blood plasma
2
Further reductions in DO will drive the VO below this com-
2
2
pensatory endpoint with cellular energy demand failing to be
met by aerobic metabolism alone with the development of an Republished with permission of Daedalus Enterprises Inc from Respi-
ensuing oxygen debt. In the absence of adequate oxygen to ratory Care, Murphy BA and Durbin CG Jr, 50(2), 2005; permission
meet cells’ energy demand, the cells of the body must rely on conveyed through Copyright Clearance Center, Inc.
anaerobic glycolysis to fill the energy “gap” left by inadequate
DO . The end product of anaerobic glycolysis is lactic acid, in shocked patients. Ketamine increases sympathetic tone in
12
2
the accumulation of which leads to a metabolic acidosis with most patients, this effect is not seen if presynaptic catechol-
elevated serum lactate. This metabolic acidosis is recognized as amine stores are depleted. The result in these situations is a net
a surrogate for systemic hypoperfusion and is used as one of myocardial depression. Miller et al observed that patients with
the triggers for massive transfusion protocols in many emer- a high shock index (SI) demonstrated a higher incidence of
gency medical systems (Figure 3). hypotension post RSI. These investigators stated “Ketamine is
considered a stable induction agent for rapid sequence induc-
FIGURE 3 Relationship between oxygen consumption (VO2) and tion; however, hypotension rates up to 24% are reported.”
18
oxygen delivery (DO ) when DO is acutely reduced by tamponade
2
2
or hemorrhage in anesthetized animals (data pooled from several There are also case reports of cardiac arrest in critically ill
studies). Note that blood lactate levels increase as soon as DO2 falls patients following the use of ketamine for RSI. 19
below a critically low value (DO crit).
2
Evidence
In a review of the literature, there is little high-quality evi-
dence. There are no meta-analyses of prospective, multicenter,
randomized controlled trials (RCTs). The evidence that exists
must be understood to be mostly retrospective, have a small
sample size, or be confounded by heterogeneity and bias. It is
for this reason that weight must be placed on the elements of
the PEEK clinical judgment tool. Presented next is a sample of
the available evidence.
Lockey et al. examined the survival of trauma patients who had
prehospital tracheal intubation without anesthesia or muscle
relaxants and found that the outcome was almost always fatal
20
(99.8%). Although this cohort are among the most severely
injured, it may also give a clue to the catastrophic effect of
PPV on the critically ill patient in the low-flow state.
(Reprinted by permission from Springer Nature Intensive Care Medi-
cine (Oxygen transport—the oxygen delivery controversy, Jean-Louis
Vincent & Daniel De Backer), COPYRIGHT 2004. Shafi et al. found an association with RSI and PPV and de-
creased survival in hypovolemic trauma patients, which was
The primary negative impact of PPV is an elevated intrathoracic worse when the patients were intubated in the prehospital set-
14
pressure (ITP) that is associated with reduced venous return, ting. “Patients intubated in the field were more likely to be
15
lower cardiac filling, and subsequent decreases in CO and hypotensive upon arrival in the Emergency Department (ED)
thus DO . This has been well understood, demonstrated, and (SBP < or = 90 mm Hg; ED 33%, pre-hospital 54%, p < 0.001),
2
published since the work carried out by Guyton in the 1950s. 16 and had worse survival (ED 45% versus pre-hospital 24%,
Figure 4 illustrates waveforms showing the effect of PPV. p < 0.001). Even after controlling for potential confounders,
pre-hospital Endotracheal Intubation (ETI) was still an inde-
The drugs used in RSI are themselves not without risk. Many pendent predictor of hypotension upon arrival in ED (OR 1.7,
protocols advise reductions in dose of induction drugs in the 95% CI 1.46 –2.09, p < 0.001) and decreased survival (OR
21
shocked state in recognition of this fact. NMBAs and opi- 0.51, 95% C.I. 0.43–0.62, p < 0.001).” The authors state in
ates induce vasodilation with a further reduction in venous the conclusion,“This may be mediated by the effect of positive
return. Ketamine has been perceived as a relatively safe drug pressure ventilation during hypovolemic states.” 21
RSI/PPV in Patients With Hemorrhagic Shock | 99