Page 96 - PJ MED OPS Handbook 8th Ed
P. 96
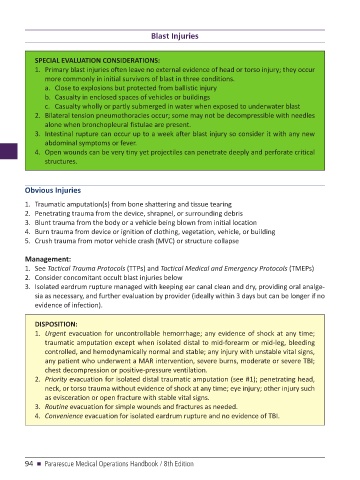
Blast Injuries
SPECIAL EVALUATION CONSIDERATIONS:
1. Primary blast injuries often leave no external evidence of head or torso injury; they occur
more commonly in initial survivors of blast in three conditions.
a. Close to explosions but protected from ballistic injury
b. Casualty in enclosed spaces of vehicles or buildings
c. Casualty wholly or partly submerged in water when exposed to underwater blast
2. Bilateral tension pneumothoracies occur; some may not be decompressible with needles
alone when bronchopleural fistulae are present.
3. Intestinal rupture can occur up to a week after blast injury so consider it with any new
abdominal symptoms or fever.
4. Open wounds can be very tiny yet projectiles can penetrate deeply and perforate critical
structures.
Obvious Injuries
1. Traumatic amputation(s) from bone shattering and tissue tearing
2. Penetrating trauma from the device, shrapnel, or surrounding debris
3. Blunt trauma from the body or a vehicle being blown from initial location
4. Burn trauma from device or ignition of clothing, vegetation, vehicle, or building
5. Crush trauma from motor vehicle crash (MVC) or structure collapse
Management:
1. See Tactical Trauma Protocols (TTPs) and Tactical Medical and Emergency Protocols (TMEPs)
2. Consider concomitant occult blast injuries below
3. Isolated eardrum rupture managed with keeping ear canal clean and dry, providing oral analge-
sia as necessary, and further evaluation by provider (ideally within 3 days but can be longer if no
evidence of infection).
DISPOSITION:
1. Urgent evacuation for uncontrollable hemorrhage; any evidence of shock at any time;
traumatic amputation except when isolated distal to mid-forearm or mid-leg, bleeding
controlled, and hemodynamically normal and stable; any injury with unstable vital signs,
any patient who underwent a MAR intervention, severe burns, moderate or severe TBI;
chest decompression or positive-pressure ventilation.
2. Priority evacuation for isolated distal traumatic amputation (see #1); penetrating head,
neck, or torso trauma without evidence of shock at any time; eye injury; other injury such
as evisceration or open fracture with stable vital signs.
3. Routine evacuation for simple wounds and fractures as needed.
4. Convenience evacuation for isolated eardrum rupture and no evidence of TBI.
94 n Pararescue Medical Operations Handbook / 8th Edition