Page 102 - PJ MED OPS Handbook 8th Ed
P. 102
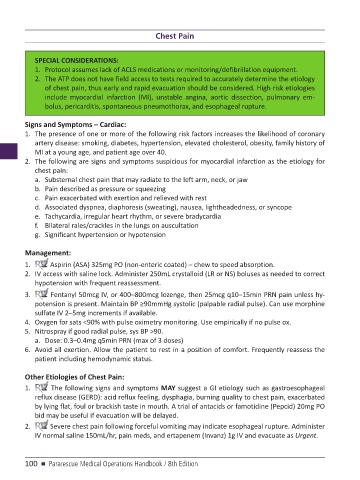
Chest Pain
SPECIAL CONSIDERATIONS:
1. Protocol assumes lack of ACLS medications or monitoring/defibrillation equipment.
2. The ATP does not have field access to tests required to accurately determine the etiology
of chest pain, thus early and rapid evacuation should be considered. High risk etiologies
include myocardial infarction (MI), unstable angina, aortic dissection, pulmonary em-
bolus, pericarditis, spontaneous pneumothorax, and esophageal rupture.
Signs and Symptoms – Cardiac:
1. The presence of one or more of the following risk factors increases the likelihood of coronary
artery disease: smoking, diabetes, hypertension, elevated cholesterol, obesity, family history of
MI at a young age, and patient age over 40.
2. The following are signs and symptoms suspicious for myocardial infarction as the etiology for
chest pain:
a. Substernal chest pain that may radiate to the left arm, neck, or jaw
b. Pain described as pressure or squeezing
c. Pain exacerbated with exertion and relieved with rest
d. Associated dyspnea, diaphoresis (sweating), nausea, lightheadedness, or syncope
e. Tachycardia, irregular heart rhythm, or severe bradycardia
f. Bilateral rales/crackles in the lungs on auscultation
g. Significant hypertension or hypotension
Management:
1. Aspirin (ASA) 325mg PO (non-enteric coated) – chew to speed absorption.
2. IV access with saline lock. Administer 250mL crystalloid (LR or NS) boluses as needed to correct
hypotension with frequent reassessment.
3. Fentanyl 50mcg IV, or 400–800mcg lozenge, then 25mcg q10–15min PRN pain unless hy-
potension is present. Maintain BP ≥90mmHg systolic (palpable radial pulse). Can use morphine
sulfate IV 2–5mg increments if available.
4. Oxygen for sats <90% with pulse oximetry monitoring. Use empirically if no pulse ox.
5. Nitrospray if good radial pulse, sys BP >90.
a. Dose: 0.3–0.4mg q5min PRN (max of 3 doses)
6. Avoid all exertion. Allow the patient to rest in a position of comfort. Frequently reassess the
patient including hemodynamic status.
Other Etiologies of Chest Pain:
1. The following signs and symptoms MAY suggest a GI etiology such as gastroesophageal
reflux disease (GERD): acid reflux feeling, dysphagia, burning quality to chest pain, exacerbated
by lying flat, foul or brackish taste in mouth. A trial of antacids or famotidine (Pepcid) 20mg PO
bid may be useful if evacuation will be delayed.
2. Severe chest pain following forceful vomiting may indicate esophageal rupture. Administer
IV normal saline 150mL/hr, pain meds, and ertapenem (Invanz) 1g IV and evacuate as Urgent.
100 n Pararescue Medical Operations Handbook / 8th Edition