Page 105 - JSOM Spring 2024
P. 105
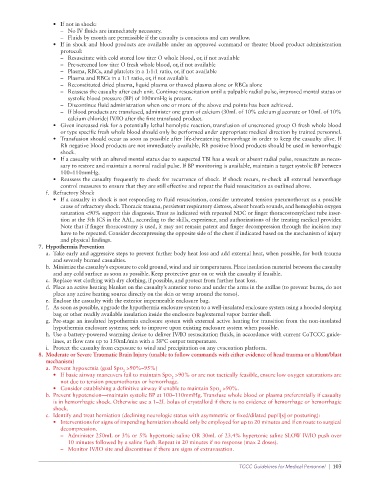
• If not in shock:
– No IV fluids are immediately necessary.
– Fluids by mouth are permissible if the casualty is conscious and can swallow.
• If in shock and blood products are available under an approved command or theater blood product administration
protocol:
– Resuscitate with cold stored low titer O whole blood, or, if not available
– Pre-screened low titer O fresh whole blood, or, if not available
– Plasma, RBCs, and platelets in a 1:1:1 ratio, or, if not available
– Plasma and RBCs in a 1:1 ratio, or, if not available
– Reconstituted dried plasma, liquid plasma or thawed plasma alone or RBCs alone
– Reassess the casualty after each unit. Continue resuscitation until a palpable radial pulse, improved mental status or
systolic blood pressure (BP) of 100mmHg is present.
– Discontinue fluid administration when one or more of the above end points has been achieved.
– If blood products are transfused, administer one gram of calcium (30mL of 10% calcium gluconate or 10mL of 10%
calcium chloride) IV/IO after the first transfused product.
• Given increased risk for a potentially lethal hemolytic reaction, transfusion of unscreened group O fresh whole blood
or type specific fresh whole blood should only be performed under appropriate medical direction by trained personnel.
• Transfusion should occur as soon as possible after life-threatening hemorrhage in order to keep the casualty alive. If
Rh negative blood products are not immediately available, Rh positive blood products should be used in hemorrhagic
shock.
• If a casualty with an altered mental status due to suspected TBI has a weak or absent radial pulse, resuscitate as neces-
sary to restore and maintain a normal radial pulse. If BP monitoring is available, maintain a target systolic BP between
100–110mmHg.
• Reassess the casualty frequently to check for recurrence of shock. If shock recurs, re-check all external hemorrhage
control measures to ensure that they are still effective and repeat the fluid resuscitation as outlined above.
f. Refractory Shock
• If a casualty in shock is not responding to fluid resuscitation, consider untreated tension pneumothorax as a possible
cause of refractory shock. Thoracic trauma, persistent respiratory distress, absent breath sounds, and hemoglobin oxygen
saturation <90% support this diagnosis. Treat as indicated with repeated NDC or finger thoracostomy/chest tube inser-
tion at the 5th ICS in the AAL, according to the skills, experience, and authorizations of the treating medical provider.
Note that if finger thoracostomy is used, it may not remain patent and finger decompression through the incision may
have to be repeated. Consider decompressing the opposite side of the chest if indicated based on the mechanism of injury
and physical findings.
7. Hypothermia Prevention
a. Take early and aggressive steps to prevent further body heat loss and add external heat, when possible, for both trauma
and severely burned casualties.
b. Minimize the casualty’s exposure to cold ground, wind and air temperatures. Place insulation material between the casualty
and any cold surface as soon as possible. Keep protective gear on or with the casualty if feasible.
c. Replace wet clothing with dry clothing, if possible, and protect from further heat loss.
d. Place an active heating blanket on the casualty’s anterior torso and under the arms in the axillae (to prevent burns, do not
place any active heating source directly on the skin or wrap around the torso).
e. Enclose the casualty with the exterior impermeable enclosure bag.
f. As soon as possible, upgrade the hypothermia enclosure system to a well-insulated enclosure system using a hooded sleeping
bag or other readily available insulation inside the enclosure bag/external vapor barrier shell.
g. Pre-stage an insulated hypothermia enclosure system with external active heating for transition from the non-insulated
hypothermia enclosure systems; seek to improve upon existing enclosure system when possible.
h. Use a battery-powered warming device to deliver IV/IO resuscitation fluids, in accordance with current CoTCCC guide-
lines, at flow rate up to 150mL/min with a 38°C output temperature.
i. Protect the casualty from exposure to wind and precipitation on any evacuation platform.
8. Moderate or Severe Traumatic Brain Injury (unable to follow commands with either evidence of head trauma or a blunt/blast
mechanism)
a. Prevent hypoxemia (goal Spo >90%–95%)
2
• If basic airway maneuvers fail to maintain Spo >90% or are not tactically feasible, ensure low oxygen saturations are
2
not due to tension pneumothorax or hemorrhage.
• Consider establishing a definitive airway if unable to maintain Spo >90%.
2
b. Prevent hypotension—maintain systolic BP at 100–110mmHg. Transfuse whole blood or plasma preferentially if casualty
is in hemorrhagic shock. Otherwise use a 1–2L bolus of crystalloid if there is no evidence of hemorrhage or hemorrhagic
shock.
c. Identify and treat herniation (declining neurologic status with asymmetric or fixed/dilated pupil[s] or posturing):
• Interventions for signs of impending herniation should only be employed for up to 20 minutes and if en route to surgical
decompression.
– Administer 250mL or 3% or 5% hypertonic saline OR 30mL of 23.4% hypertonic saline SLOW IV/IO push over
10 minutes followed by a saline flush. Repeat in 20 minutes if no response (max 2 doses).
– Monitor IV/IO site and discontinue if there are signs of extravasation.
TCCC Guidelines for Medical Personnel | 103