Page 20 - Journal of Special Operations Medicine - Summer 2015
P. 20
hypothalamus, adrenal gland, and pituitary gland. The released into the bloodstream to regulate metabolic, car-
hypothalamus is located inferior to the thalamus and diovascular, immune, and behavioral processes. When
18
superior to the brainstem. The pituitary gland is located sufficient glucocorticoids are detected in the body, the
inferior to the hypothalamus and connected to it via the hypothalamus inhibits the production of CRF through
infundibulum. The pituitary gland has a posterior lobe two mechanisms. The first is not fully understood, but
and an anterior lobe. The posterior lobe is composed regulation may occur through sensing the rate at which
of the infundibulum and pars nervosa, and the anterior glucocorticoids are secreted. The second system is the
18
lobe is composed of the pars tuberalis in the superior traditional HPA feedback, which is well known. Gluco-
region and the pars distalis in the inferior portion. The corticoids bind with receptors in the PNV and possibly
adrenal glands are located just superior to the kidneys in the hippocampus, allowing for modification of the
and measure approximately 5cm vertically, 3cm wide, HPA. Thus, the HPA axis is a negative feedback system.
18
and 1cm from anterior to posterior. They also are com-
posed of two parts: the adrenal cortex and the adrenal The body naturally produces cortisol as a stress re-
medulla. The adrenal cortex comprises three regions: sponse to inflammation. In some cases, steroidal anti-
the zona glomerulosa, the zona fasciculata, and the zona inflammatory medications are given to alleviate swelling.
reticularis. 17 They alleviate the inflammation by inhibiting the release
of arachidonic acid from the plasma membrane, which
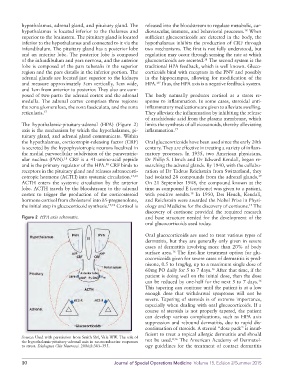
The hypothalamic-pituitary-adrenal (HPA) (Figure 2) limits the synthesis of all eicosanoids, thereby alleviating
axis is the mechanism by which the hypothalamus, pi- inflammation. 17
tuitary gland, and adrenal gland communicate. Within
the hypothalamus, corticotropin-releasing factor (CRF) Oral glucocorticoids have been used since the early 20th
is secreted by the hypophysiotropic neurons localized in century. They are effective in treating a variety of inflam-
the medial parvocellular subdivision of the paraventric- matory processes. In 1935, two American physicians,
ular nucleus (PVN). CRF is a 41-amino-acid peptide Dr Philip S. Hench and Dr Edward Kendall, began re-
18
and is the primary regulator of the HPA. CRF binds to searching the adrenal glands. By 1940, with the collabo-
18
receptors in the pituitary gland and releases adrenocorti- ration of Dr Tadeus Reichstein from Switzer land, they
cotropic hormone (ACTH) into systemic circulation. 17,18 had isolated 28 compounds from the adrenal glands.
19
ACTH enters the systemic circulation by the anterior On 21 September 1948, the compound known at the
lobe. ACTH travels by the bloodstream to the adrenal time as compound E (cortisone) was given to a patient,
cortex to trigger the production of the corticosteroid with positive results. In 1950, Drs Hench, Kendall,
19
hormone cortisol from cholesterol into δ5-pregnenolone, and Reichstein were awarded the Nobel Prize in Physi-
the initial step in glucocorticoid synthesis. 17,18 Cortisol is ology and Medicine for the discovery of cortisone. The
19
discovery of cortisone provided the required research
Figure 2 HPA axis schematic. and base structure needed for the development of the
oral glucocorticoids used today.
Oral glucocorticoids are used to treat various types of
dermatitis, but they are generally only given in severe
cases of dermatitis involving more than 20% of body
surface area. The first-line treatment option for glu-
16
cocorticoids given for severe cases of dermatitis is pred-
nisone, 0.5 to 1mg/kg, up to a maximum single dose of
60mg PO daily for 5 to 7 days. After that time, if the
16
patient is doing well on the initial dose, then the dose
can be reduced by one-half for the next 5 to 7 days. 16
This tapering can continue until the patient is at a low
enough dose that withdrawal symptoms will not be
severe. Tapering of steroids is of extreme importance,
especially when dealing with oral glucocorticoids. If a
course of steroids is not properly tapered, the patient
can develop various complications, such as HPA axis
suppression and rebound dermatitis, due to rapid dis-
continuation of steroids. A steroid “dose pack” is insuf-
ficient to treat a topical allergic dermatitis and should
Source: Used with permission from Smith SM, Vale WW. The role of 8,16
the hypothalamic-pituitary-adrenal axis in neuroendocrine responses not be used. The American Academy of Dermatol-
to stress. Dialogues Clin Neurosci. 2006;8:383–395. ogy guidelines for the treatment of contact dermatitis
10 Journal of Special Operations Medicine Volume 15, Edition 2/Summer 2015